Nearly 18 months after the COVID-19 pandemic began, and six months after safe and effective vaccines became available, the U.S. is facing another surge in cases. How is it possible that, as of July 17, COVID-19 infections were increasing in nearly all 50 states?
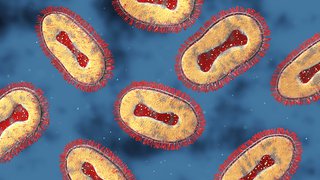
The highly transmissible delta variant, which is now the predominant strain of the virus here, is spreading quickly and mostly among the unvaccinated. In fact, more than 97 percent of patients entering the hospital are unvaccinated, according to CDC Director Rochelle Walensky, who also noted: “This is becoming a pandemic of the unvaccinated.”
Even though 56 percent of Americans have received at least one dose of vaccine and 161 million (49 percent) are fully vaccinated, the virus will continue to do what viruses do – search for available hosts, spread, and mutate – as long as a large portion of our population delays or avoids getting vaccinated. And that puts everyone at risk.
So, is there anything you can say to a reluctant friend or family member to persuade them that vaccination is the right choice for them?
The short answer is: Yes. A poll released recently by the Kaiser Family Foundation found that about one-fifth of Americans who said in January they were hesitant about or dead-set against getting a COVID-19 vaccine have since gotten their shots. Many said family, friends, and doctors helped change their minds. The poll also identified some primary reasons people are still avoiding vaccinations.
Let’s examine those and provide science-backed explanations that might potentially sway their thinking – and help put an end to the pandemic once and for all.
Responses to top 10 COVID-19 vaccine concerns
1. 'I'm concerned about side effects, particularly long term'
Unlike some medications we take daily, which can build up in the body, vaccines are essentially a one-and-done treatment that gets eliminated quickly. They are designed to deliver a payload, provoke immunity, and degrade. Even with a booster shot, the messenger RNA (mRNA) in the Pfizer and Moderna COVID-19 vaccines works incredibly fast – it signals cells to make copies of the spike protein and triggers an immune response, and then natural enzymes break down the mRNA within a few days.
Because of this, any side effects from the vaccines usually surface quickly – sore arm, headache, fatigue – and only last a day or two. If there is going to be a serious side effect, it will almost certainly come within two weeks to two months of the rollout of a vaccine, which has proven to be true throughout our long history with vaccinations. For the COVID-19 vaccines, Phase 3 clinical trials followed thousands of people for 60 days post-vaccination before safety data could be submitted.
Further, the V-safe After Vaccination Health Checker has created the most extensive long-term monitoring database of post-vaccine effects ever. The vaccines have been proven safe and effective in both the clinical trials and through this long-term monitoring effort.
2. 'The vaccines were rushed and remain authorized only for emergency use'
The COVID-19 vaccines were put through the same rigorous testing that faces any new drug seeking authorization by the U.S. Food and Drug Administration (FDA). The only thing that was accelerated or eliminated were some of the administrative processes – the red tape that can sometimes slow down approvals. Also, rather than do the studies in succession, clinical trials were conducted in tandem (at the same time) allowing the same amount of research to be completed in a shorter time.
The vaccines were granted “emergency use authorization” because they were developed during a devastating and deadly public health crisis. Full FDA approval, which requires a review of six months’ worth of data, will confirm what we already know: The vaccines are safe and very effective. Pfizer submitted its request for full FDA approval in May and it is progressing (on July 16 it earned approval for its biologics license); Moderna’s was filed in June. You should not wait for this formality to get vaccinated.
3. 'I never get sick. My immune system will protect me from COVID-19'
SARS-CoV-2 is a novel coronavirus, which means your immune system – no matter how strong – has no existing antibodies to mount a defense against it unless you’ve already had COVID-19. Certainly, immune systems vary based on genetics, age, diet, exercise habits, and even exposure to past pathogens, but COVID-19 has proven itself to be very unpredictable, exacting a toll on people of all ages.
Some people may even be victims of their strong immune systems. COVID-19 has sparked what’s called a cytokine storm in some patients, which is essentially an overreaction of the immune system that causes severe inflammation in vital organs such as the heart and lungs.
The safest way to strengthen your immune system against a novel coronavirus is to get vaccinated.
4. 'I'm worried the mRNA vaccines will change my DNA'
The mRNA in the vaccines never enters the nucleus of your cells, where DNA lives, so it cannot affect your DNA.
Essentially, mRNA is a technology that the vaccines use to show your immune system the genetic code for the SARS-CoV-2 spike protein, so when your body encounters the virus in real life it recognizes the invader and mounts a defense.
The mRNA does not affect your DNA, and it remains in your body for only a few days.
5. 'The vaccine will affect my fertility'
There is no medical or scientific way for the COVID-19 vaccines to interact with the female reproductive organs. This bit of misinformation is rooted in a disproven theory that because the SARS-CoV-2 spike protein resembles the syncytin-1 protein crucial for formation of the placenta, the vaccines might target them. Virologists have said the proteins are nowhere near similar enough to confuse antibodies or cause infertility. Take the time to correct anyone who spreads that rumor.
Preliminary research has shown the vaccines are safe for pregnant women and may provide some protective antibodies for their newborns.
As for fertility in men, the vaccines won’t cause any adverse effects, but a recently published journal review suggests COVID-19 infection might have a negative impact on testicular function and sperm production.
6. 'The virus and delta variant don’t pose a real threat to young people'

The biggest increase in cases recently has been among unvaccinated people ages 29 to 40. Hospitalizations among that age group also have been on the rise.
Data indicate that vaccinated people are largely protected from serious illness from the delta variant, which is considered highly infectious and more transmissible than the original SARS-CoV-2 virus. It also appears to cause more severe disease, particularly in the unvaccinated. The risk of hospitalization increases two-fold if you’re infected with the delta variant.
While deaths from COVID-19 are rare among young people, they are susceptible to “long-haul COVID” complications such as respiratory problems, loss of smell, and brain fog. A study published in JAMA Network Open in February said that 30 percent of people who had COVID-19 continue to have symptoms up to nine months after infection. Although we are still studying these long-term symptoms, we know getting vaccinated will prevent these health effects.
7. 'I’ve had COVID-19, so I have natural immunity and don’t need a vaccine'
Recent studies have shown that protection provided by COVID-19 vaccines is robust and longer-lasting than natural immunity. There have also been reported cases of people who have had COVID-19 and been reinfected, so experts recommend vaccination, particularly for added protection against variants.
8. 'Getting the vaccine is a hassle. I can’t take time off work to wait in line'
COVID-19 vaccines are now widely available – from retail pharmacies (Walgreens, CVS) to grocery stores (Kroger, Albertson’s) to big box outlets (Walmart, Target). You can also get one at your doctor’s office or an outpatient clinic such as at UT Southwestern. The CDC has an easy-to-use vaccine finder online to get locations near you, or you can call 1-800-232-0233. You can even text your ZIP code to 438839.
9. 'I don’t want to be a guinea pig'
Vaccine hesitancy runs deeps, particularly in communities of color where historical abuses and limited access to health care continue to stoke distrust. But many doctors, nurses, scientists, and health care workers of color – including many at UT Southwestern – have publicly endorsed the safety of the COVID-19 vaccines by posting photos and videos of themselves getting vaccinated.
Unfortunately, COVID-19 and its treatments have been entangled in politics, fostering mistrust. Just as you would with any other disease, talk to your doctor about your concerns and bring your questions to your appointment.
Frontline workers were among the first people to get vaccinated in December 2020, and since then more than 1 billion people worldwide have gotten their shots. This is not an experiment, it is an unprecedented scientific “win” that we learned how to prevent a terrible disease just months after its discovery. Vaccines, and these in particular, are the best medicine has to offer – disease prevention.
10. 'I just want more time and proof the vaccines are safe'
More than 300 million doses of the COVID-19 vaccines have been delivered in the U.S. as of July 17, and the number of serious side effects has been miniscule.
The CDC and FDA have robust reporting systems in place to review all side effects. Whenever a pattern of adverse reactions has been detected, such as six cases of blood clots in women under 50 from the Johnson & Johnson vaccine, the agencies haven’t hesitated to take action. The J&J vaccine was paused for a week in April for review by an independent panel, which ultimately deemed it safe and the reactions extremely rare.
At UT Southwestern, we also have our own Scientific Review Committee that independently reviewed clinical trial data for the Pfizer and Moderna vaccines. We would not have offered them to our employees and patients if we had any doubts about their safety or efficacy.

Booking a COVID-19 vaccine appointment at UT Southwestern is easy and takes just a few minutes.
Avoiding vaccine puts everyone at risk
The problem with putting off or avoiding vaccination for COVID-19 is that it gives the virus time to spread and mutate, which means both vaccinated and unvaccinated people could be susceptible to future variants. It also means the pandemic – and measures such as mask mandates, in-person event cancellations, and travel restrictions – won’t end, either.
Just recently, Los Angeles County reinstated its indoor mask rules because of surging cases. The Tokyo Olympics won’t have fans. And the American Academy of Pediatrics just recommended universal masking in schools for the upcoming year because “many schools will not have a system to monitor vaccine status of students, teachers, and staff.”
Avoiding a COVID-19 vaccine is not just a choice that affects you – it puts everyone (friends, family, neighbors, co-workers) at risk. The proof is overwhelming that these vaccines are safe and effective. They are also the fastest way to finally put an end to this pandemic and to continue traveling, meeting with friends, enjoying sports and living a full, healthy life.
More in: COVID