New Nanotechnology Allows Tissue-Specific Delivery of Genomic Medicines
April 30, 2021
Research That’s Supported By the NCI
Research at the Harold C. Simmons Comprehensive Cancer Center is organized into five programs that are funded in part by a Cancer Center Support Grant from the National Cancer Institute. These complementary research programs work together to deliver Simmons Cancer Center's mission to ease the burden of cancer through ground-breaking discovery, transdisciplinary research, impactful community engagement, education, and exceptional patient care.
Researchers are combining experience in chemical synthesis and nanoparticle engineering with knowledge of the mechanisms of cancer development to design future therapies.
As a materials chemistry and engineering laboratory at UT Southwestern Medical Center, my research group is in a unique position to focus on next generation genomic medicines. In collaboration with our colleagues at the Simmons Comprehensive Cancer Center, we can quickly test them in preclinical models.
Nanoparticle Delivery of mRNA-Based Therapeutics
Novel mRNA-based therapeutics leverage a natural process that takes place in the cell: the translation of messenger RNA (mRNA) to protein. For example, mRNA delivery is the leading strategy for the SARS-CoV-2 vaccines, and recent studies have demonstrated that nucleic acids can be utilized as anti-cancer therapeutics. Furthermore, we are using nanoparticles to deliver genome editing proteins such as CRISPR-Cas and nucleic acids to cells to correct disease-causing genetic variants or mutations in DNA.
Today, there now are effective ways to use self-assembled nanoparticles for drug delivery. Similar to the functioning — and size — of a virus, synthetic nanoparticles encapsulate nucleic acids and/or proteins, internalize into cells, and release drugs. While there has been great progress in delivery of small nucleic acids to the liver, targeted delivery of cargoes to other tissues, including tumors, has seen limited progress and remains a major challenge in the field. [1] During the past eight years, we have been focused on discovering nanoparticle formulations that are capable of encapsulating small to large nucleic acids and have recently developed new chemicals that can mediate effective delivery of long nucleic acids like mRNA and gene editing proteins like Cas9.
“While there has been great progress in delivery of small nucleic acids to the liver, targeted delivery of cargoes to other tissues, including tumors, has seen limited progress and remains a major challenge in the field.”
Daniel Siegwart, Ph.D.
Selective ORgan Targeting (SORT)
Recently, we discovered a new technology that we call selective organ targeting (SORT). [2] SORT is a universal strategy to systematically engineer nanoparticles that can localize to targeted tissues (such as liver, lungs, and spleen) to deliver genomic medicines. Building upon nanoparticles that only targeted the liver for hepatocellular carcinoma (HCC) and genetic disease treatment, [3-4] we add a supplemental SORT molecule that changes how the body perceives the nanoparticles. The resulting formation of a unique endogenous identity selectively shuttles them to different tissues.
Using SORT nanoparticles, we have successfully delivered mRNAs and the molecular editing tools of CRISPR-Cas to the lungs, spleen, lymph nodes, bone marrow, and liver and edited therapeutically relevant cell types, including epithelial cells, endothelial cells, B cells, T cells, and hepatocytes in animal models. [2] We are currently working to develop SORT nanoparticles for additional organs and are optimistic that SORT will be effective for tissue-specific targeting in human beings someday as well.
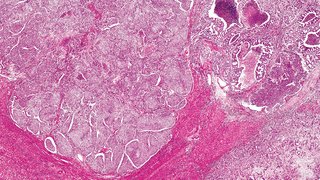
In the context of specific cancers, we are currently combining gene silencing with gene editing to create a novel combination therapy against aggressive HCC in collaboration with Professor Hao Zhu. In addition, we have used our SORT nanoparticles to rapidly create lung and liver cancer models. [5] Bypassing historical methods of mouse model generation that are laborious and long (6-12 months), we have been able to directly create cancer models in a single day by simply injecting nanoparticles intravenously. Lung-selective SORT nanoparticles can traffic to the lungs, where the CRISPR-Cas genome editing system creates targeted deletions of tumor suppressor genes or induces chromosomal changes to induce formation of a cancer-causing oncogene, mimicking a specific patient’s mutation. Building on this work, we are actively treating liver and lung cancer models using these targeted nanoparticles to test potential therapies. The SORT technology has been licensed to a UTSW spinout company called ReCode Therapeutics, who anticipates beginning clinicals trials by 2022 for multiple pulmonary diseases.
Creating CAR T Cells In Situ
Chimeric antigen receptor (CAR) T cell therapy is a powerful immunotherapy approach, whereby a patient's T cells are taken from their blood and genetically engineered in a specialized laboratory to express a CAR that can specifically target the patient’s cancer. The CAR T cells are then expanded in cell culture and shipped back to the hospital where they are infused into the patient. It is a very effective therapy for cancers such as B-cell acute lymphoblastic leukemia. However, shipping the blood to the laboratory and engineering the cells presents logistical challenges. Additionally, the process is expensive and time consuming when every moment counts for a patient with active cancer.
To address these challenges, we are investigating SORT nanoparticles that may be able to carry CRISPR-Cas to create CAR T cells in situ (directly in the body). In this potential future therapy, nanoparticles would be administered directly into the blood, where they would traffic to T cells in the spleen, lymph nodes, and bone marrow, and use CRISPR-Cas to insert the appropriate CAR. This is a work in progress undergoing initial testing in animal models. But if it proves to be safe and effective, the long-term vision is to replace the timely and expensive processes currently used in T cell engineering.
Our overall advances in materials science and engineering have enabled us to deliver therapeutic nucleic acid drugs including siRNA, miRNA, tRNA, mRNA, pDNA, and CRISPR/Cas to models of liver, ovarian, breast, and lung cancer. [2-3, 5-10] We are currently focused on expanding the SORT molecule repertoire for targeted access additional tissues, determining underlying mechanisms of action, and working towards the ultimate goal of developing genomic medicines to treat a variety of cancer types and genetic disorders.
About the Author
Daniel J. Siegwart, Ph.D., is an Associate Professor in the Department of Biochemistry and the Simmons Cancer Center at UT Southwestern Medical Center. The central goal of the Siegwart Research Group is to use materials chemistry to solve challenges in disease therapy and diagnosis. In particular, they are focused on the development of new materials that can deliver ribonucleic acids (RNAs) to improve cancer outcomes.
Footnotes
1. Wei, T.; Cheng, Q.; Farbiak, L.; Anderson, D. G.; Langer, R.; Siegwart, D. J., Delivery of tissue-targeted scalpels: Opportunities and challenges for in vivo CRISPR/Cas-based genome editing. ACS Nano 2020, 14 (8), 9243-9262.
2. Cheng, Q.; Wei, T.; Farbiak, L.; Johnson, L. T.; Dilliard, S. A.; Siegwart, D. J., Selective ORgan Targeting (SORT) nanoparticles for tissue specific mRNA delivery and CRISPR/Cas gene editing. Nat. Nanotechnol. 2020, 15 (4), 313-320.
3. Zhou, K.; Nguyen, L. H.; Miller, J. B.; Yan, Y.; Kos, P.; Xiong, H.; Li, L.; Hao, J.; Minnig, J. T.; Zhu, H.; Siegwart, D. J., Modular degradable dendrimers enable small RNAs to extend survival in an aggressive liver cancer model. Proc. Natl. Acad. Sci. U.S.A. 2016, 113 (3), 520-525.
4. Cheng, Q.; Wei, T.; Jia, Y.; Farbiak, L.; Zhou, K.; Zhang, S.; Wei, Y.; Zhu, H.; Siegwart, D. J., Dendrimer-based lipid nanoparticles deliver therapeutic FAH mRNA to normalize liver function and extend survival in a mouse model of hepatorenal tyrosinemia type I. Adv. Mater. 2018, 30 (52), e1805308.
5. Wei, T.; Cheng, Q.; Min, Y. L.; Olson, E. N.; Siegwart, D. J., Systemic nanoparticle delivery of CRISPR-Cas9 ribonucleoproteins for effective tissue specific genome editing. Nat. Commun. 2020, 11 (1), 3232.
6. Yan, Y.; Liu, L.; Xiong, H.; Miller, J. B.; Zhou, K.; Kos, P.; Huffman, K. E.; Elkassih, S.; Norman, J. W.; Carstens, R.; Kim, J.; Minna, J. D.; Siegwart, D. J., Functional polyesters enable selective siRNA delivery to lung cancer over matched normal cells. Proc. Natl. Acad. Sci. U.S.A. 2016, 113 (39), E5702-E5710.
7. Miller, J. B.; Zhang, S.; Kos, P.; Xiong, H.; Zhou, K.; Perelman, S. S.; Zhu, H.; Siegwart, D. J., Non-viral CRISPR/Cas gene editing in vitro and in vivo enabled by synthetic nanoparticle co-delivery of Cas9 mRNA and sgRNA. Angew. Chem. Int. Ed. 2017, 56 (4), 1059-1063.
8. Xiong, H.; Zuo, H.; Yan, Y.; Occhialini, G.; Zhou, K.; Wan, Y.; Siegwart, D. J., High-contrast fluorescence detection of metastatic breast cancer including bone and liver micrometastases via size-controlled pH-activatable water-soluble probes. Adv. Mater. 2017, 29 (29), 1700131.
9. Yan, Y.; Zhou, K.; Xiong, H.; Miller, J. B.; Motea, E. A.; Boothman, D. A.; Liu, L.; Siegwart, D. J., Aerosol delivery of stabilized polyester-siRNA nanoparticles to silence gene expression in orthotopic lung tumors. Biomaterials 2017, 118, 84-93.
10. Xiong, H.; Liu, S.; Wei, T.; Cheng, Q.; Siegwart, D. J., Theranostic dendrimer-based lipid nanoparticles containing PEGylated BODIPY dyes for tumor imaging and systemic mRNA delivery in vivo. J. Controlled Release 2020, 325, 198-205.