What Is Percutaneous Coronary Intervention?
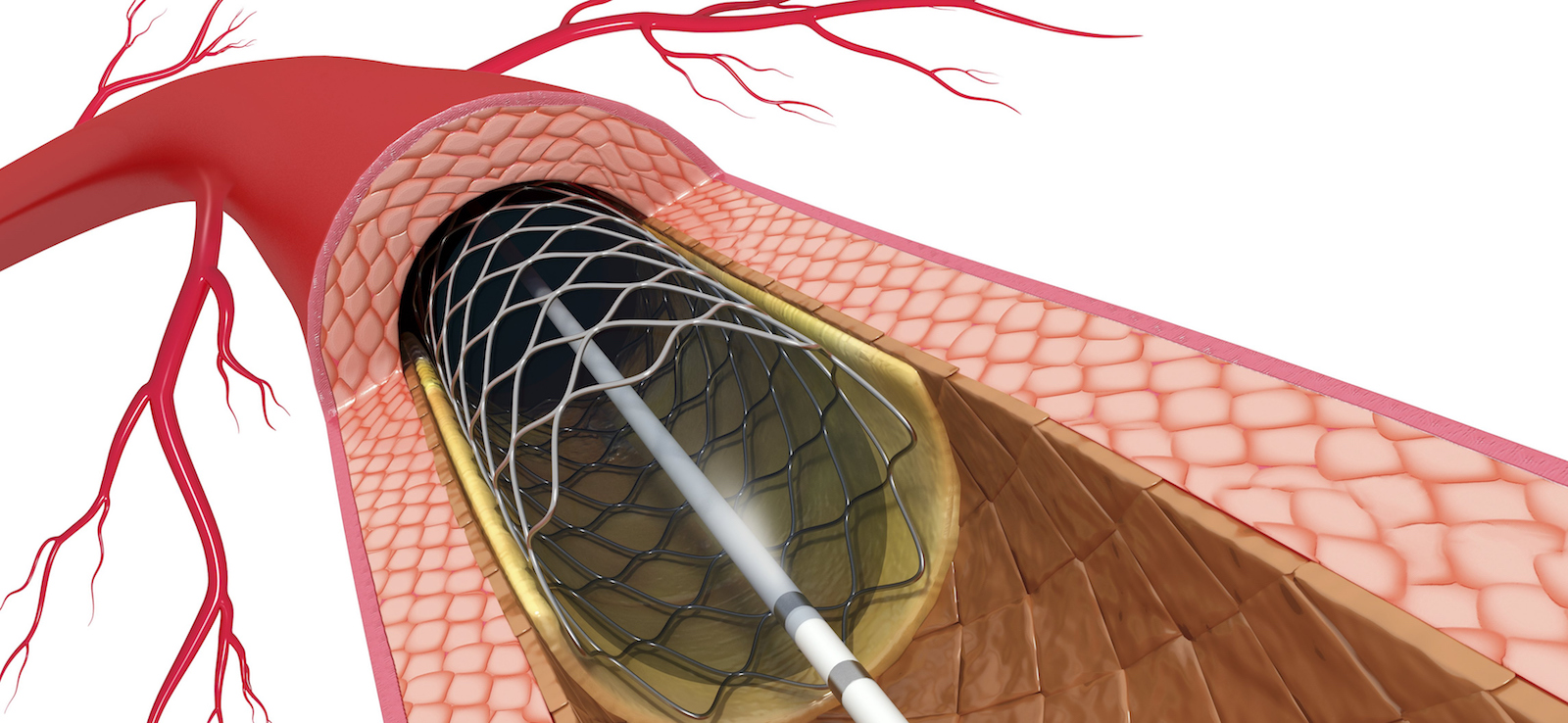
Percutaneous coronary intervention (PCI) is a minimally invasive procedure that opens narrowed or blocked coronary (heart) arteries. In a PCI, doctors are able to perform angioplasty (a procedure to repair or open a blood vessel) and place stents (tiny, metal mesh tubes inserted into blood vessels to keep them open).
The Comprehensive Heart and Vascular Center at UT Southwestern is one of the country’s leading cardiovascular programs, with experts who are at the forefront of the latest research to treat atherosclerosis and coronary artery disease. We offer our patients extensive experience in minimally invasive heart procedures to provide safe, effective care with faster recovery times than traditional surgery allows.
What Conditions Are Treated with Percutaneous Coronary Interventions?
When excess cholesterol and other fats build up in the bloodstream, they can collect inside artery walls. This buildup is called plaque, and it causes a condition known as atherosclerosis.
PCI can treat conditions that result from atherosclerosis, such as:
How Is a Percutaneous Coronary Intervention Performed?
In a PCI, the doctor makes a tiny incision, usually in the wrist, to access an artery with a sheath (similar to an IV). Through this sheath, doctors then insert a catheter (a thin, flexible tube) that is carefully threaded to the heart using live imaging as guidance. Doctors then perform coronary angiography (pictures of the coronary arteries) to identify any areas of atherosclerosis.
The doctor then inserts a tiny balloon using the catheter and guides it to the blocked area of the artery. Inflating the balloon presses the plaque against the artery walls, opening the vessel to allow blood flow. In certain situations, additional advanced techniques are needed to adequately prepare the vessel for coronary stent placement.
At UT Southwestern, our interventional cardiologists are able to perform several advanced techniques during PCI:
- Coronary (intravascular) lithotripsy: Doctors use sonic pressure waves to fracture calcified plaques in the coronary arteries to allow for more effective stent deployment and improve blood flow.
- Laser angioplasty: Doctors use a laser-tipped catheter, instead of a balloon, to open the artery by sending beams of light to vaporize the blockage.
- Rotational atherectomy: Doctors use a catheter with an abrasive tip to remove plaque from an artery by essentially “sanding” it off artery walls. The abrasive tip grinds plaque into microscopic particles to avoid creating another blockage further downstream.
- Orbital atherectomy: This atherectomy technique uses an abrasive “crown,” a circular section on the catheter that spins around the wire to remove plaque from artery walls. Orbital atherectomy also grinds plaque into microscopic particles.
- Coronary brachytherapy: This procedure for patients with multiple stents or recurring stent narrowing (in-stent restenosis) involves the placement of radioactive material into the coronary artery to deliver focal radiation to the affected area; the radiation prevents scar tissue from growing and the artery from narrowing.
- Coronary drug-coated balloon angioplasty: Doctors use these specialized coronary artery balloons to perform angioplasty on patients with multiple stents or recurring in-stent restenosis and simultaneously deliver antiproliferative drugs to the coronary artery wall, which can improve long-term vessel patency.
After the vessel has been prepared, a coronary stent is usually placed to hold the vessel open. A drug-eluting stent slowly releases medication over time. It helps prevent scar tissue from forming and reduces the risk of future blockages.
What Can Patients Expect During Percutaneous Coronary Intervention?
Pre-Procedure Details
The surgeon provides specific instructions to the patient before the PCI and explains risks such as bleeding, infection, or adverse reaction to anesthesia.
Patients should follow the instructions provided by their provider before the procedure.
On the day of surgery, the patient arrives at the hospital, registers, and changes into a hospital gown. A nurse reviews the patient’s charts to ensure there are no problems.
Patients receive moderate sedation when they arrive at the operating room, where the surgeon verifies the patient’s name and procedure before any medication is given. The procedure begins once the sedation is in effect.
Post-Procedure Details
After the procedure, patients are taken to the postoperative recovery area and monitored.
The length of the hospital stay depends on how quickly the patient is able to recover and perform some physical activity. In many cases, patients can go home the same day.
What Support Services Does UT Southwestern Offer?
UT Southwestern’s cardiac rehabilitation specialists create customized plans that integrate proper nutrition, exercise, and, if necessary, nicotine cessation into patients’ lifestyles to improve their cardiovascular health.
What Clinical Trials Are Available for Percutaneous Coronary Intervention?
As one of the nation’s top academic medical centers, UT Southwestern offers a number of clinical trials aimed at improving the outcomes of patients with cardiovascular disease.
Clinical trials often give patients access to leading-edge treatments that are not yet widely available. Eligible patients who choose to participate in one of UT Southwestern’s clinical trials might receive treatments years before they are available to the public.