
There’s good news and bad news regarding hypertension in America. Based on the latest guidelines from the American College of Cardiology, an estimated 103 million of us – that is, nearly half of all U.S. adults – have hypertension, better known as high blood pressure (BP). Hypertension is very much a silent killer. It can go unrecognized for years until the moment a person develops organ damage, has a heart attack or stroke, or even suffers cardiovascular death.
While hypertension is not generally curable, the good news is that it’s a risk factor that can be modified. In other words, treating hypertension can prevent complications and allow a person to live a longer, healthier life.
We all need to be aware of our blood pressure, and one of the best ways to stay on top of it is through home blood pressure monitoring.
Why home BP monitoring is the way to go
In order to successfully manage high BP, we need to know our true BP numbers. Because BP fluctuates throughout the day – sometimes wildly and sometimes minute by minute – getting our BP checked only once a year at, say, our annual physical is not enough and can actually result in mismanagement.
Too many things can affect a single BP reading taken on a single day at that annual physical – bad traffic en route to the appointment or somebody cutting you off, problems with parking, having to wait too long for the doctor to see you, etc. – and all of these factors can and often do affect your BP.
There is also the very real, well-documented phenomenon known as “white coat syndrome,” which is a spike in BP that occurs from fear or anxiety when BP is taken in a clinical setting. This syndrome results in an inflated BP reading, which can lead to overtreatment on the part of the doctor writing the prescription if it is not recognized. (The opposite can also be true, which is the case in “masked hypertension” – BP is lower in the clinic than it is at home, which can lead to undertreatment of blood pressure.)
Compare those one-off scenarios with home BP monitoring, conducted at leisure in the comfort of your own home. We encourage our patients to keep a BP log at home so we can follow trends in blood pressure rather than rely on an isolated reading. They should bring the home readings to clinic with them – and we prefer they bring their home BP monitor as well, so we can confirm its accuracy against our clinic machine and answer any questions they might have about how to use the device. We can then review the BP log with them in the clinic, which provides us with better information on which to base treatment recommendations.
“While hypertension is not generally curable, the good news is that it’s a risk factor that can be modified. In other words, treating hypertension can prevent complications and allow a person to live a longer, healthier life.”
What should the home BP numbers be?
Studies have shown that adverse cardiac events such as heart attack, stroke, and heart failure correlate better with home BP numbers than in-clinic BP numbers. For this reason, the American College of Cardiology and the American Heart Association have emphasized the importance of home BP monitoring, but the optimal home BP goal has not been well established. However, a recent study led by my UT Southwestern colleague Wanpen Vongpatanasin, M.D., has shed some light on this. She and her team found that a home BP of 130/80 mmHg correlated best with the in-clinic BP goal. (You can read about that study here.)
In short, targeting to a goal BP of less than 130/80 mmHg is the same for both home and clinic monitoring. For patients whose BP is higher than that, we should first incorporate lifestyle changes such as maintaining a healthy body weight, doing regular exercise, and limiting dietary sodium and alcohol intake to improve BP. If BP remains above the goal, the next step is to find the right medicine or medicines to help.
Don’t get frustrated
At UT Southwestern, we get a lot of referrals for patients who can’t tolerate certain BP medications or for whom nothing seems to work regarding BP management. Studies show that most people require more than one medicine – in fact, usually two or three medicines – to get to their BP goal, so it’s often a matter of figuring out what combination works best for an individual.
It’s worth noting here that even if you require two or three medications, controlling your BP does not have to be an expensive proposition. The brand-name BP drugs that are marketed so well are not necessarily any better than their generic counterparts. My practice is to simplify a patient’s medication regimen as much as possible with generic medications rather than brand-name drugs.
How to check your blood pressure at home
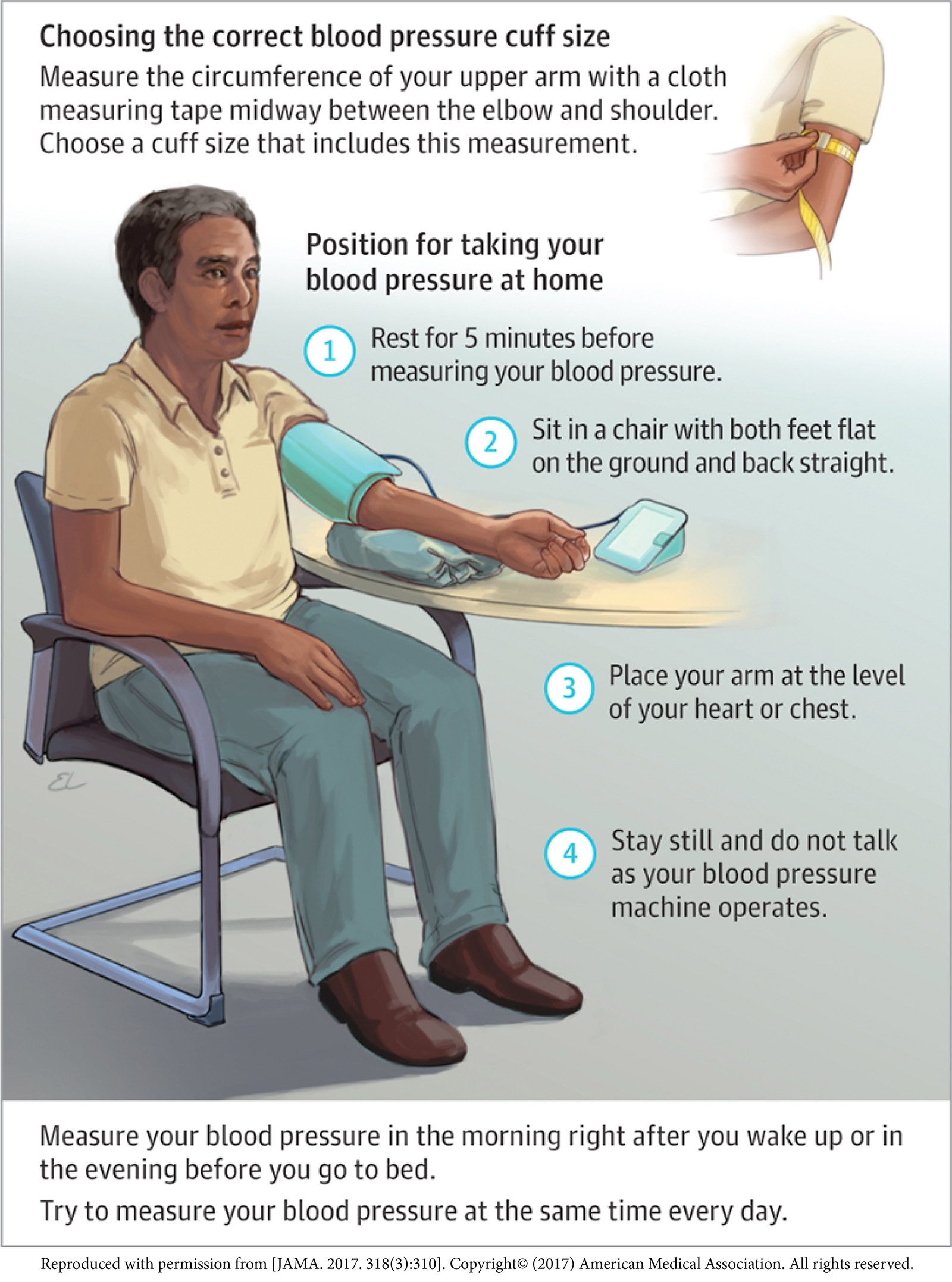
The process of taking your BP at home is pretty simple once you’ve done it a couple of times, but to make things even easier, and to supply a visual, we’ve put together a short how-to video, which you can watch here.
The first time you sit down to take your own BP, even in the comfort of your own home, the numbers you get might be higher than normal. But once you get in the routine of doing it every day – ideally at the same time and before taking any medication, making it sort of a ritual – then you’ll get used to it, and the numbers you record will reflect what’s really going on with your BP.
The video emphasizes tips for getting an accurate reading, but in a nutshell they include:
● Find a quiet place to sit with your back supported and your feet flat on the floor
● Wear the cuff on your nondominant (bare) arm and use an automatic arm cuff (wrist devices are not reliable!)
● Rest your arm at heart level and relax for about five minutes before measuring
● Don’t talk or check your cellphone or anything else – just relax
● Save the numbers to your blood pressure log
● Don’t skip a session
Who should do home BP monitoring?
The simplest answer is that I think everyone can benefit from knowing their true BP, and this can be obtained at home more accurately than in the doctor’s office. Certainly, if you’ve gone to the dentist, an obstetrician, a walk-in clinic, an emergency room, or to see any other health professional and had your BP checked and were told the reading was high, then following up with home monitoring is the right thing to do.
Knowing that hypertension is the leading modifiable risk factor for heart and vascular disease and cardiovascular death, I advise home BP monitoring for anyone who wants to be proactive about his or her health.
Think of it this way: There are many factors we can’t control that affect our health – our age, sex, family history, etc. – but BP is not one of them. BP is something we can manage if we commit to it. The point is to not wait until we have something happen to us before we start taking care of ourselves but rather to stay on top of our BP starting today.
Maintaining a home BP level of less than 130/80 mmHg should be doable. If your numbers are higher than that and lifestyle changes alone or your current medications aren’t getting you there, we can help.
To schedule an appointment with a UT Southwestern hypertension expert, call 214-645-8300 or request an appointment online.











