A year ago, Courtney White could barely walk — or even breathe. At age 23, suffering the chronic results of cystic fibrosis, her days were marked by pain, fatigue, and severe anxiety. But an extraordinary interval at UT Southwestern changed all that, and now she’s gained her second wind.
Diagnosed with cystic fibrosis at age 3, Courtney was long accustomed to the respiratory disease’s debilitating sensations — like drowning from the inside, as some have described it — along with its other unpleasant effects. But things were getting progressively worse. By mid-2012 her condition had reached the point she was spending most restless nights wondering if she was going to die in her sleep.
Courtney had spent nearly a lifetime trying to catch her breath.

In retrospect, her worries were reasonable. Even though she was equipped with portable and bedside home oxygen machines, she had still suffered a collapsed lung in late 2011, an incident that had occurred suddenly. “It felt like someone was sitting on my chest,” Courtney recalls. “I just couldn’t breathe.”
Her mom’s 911 call that night got Courtney to UT Southwestern’s St. Paul University Hospital, where doctors were able to reinflate the lung.
Courtney was put on the list for a lung transplant, but because she was petite to a fault and underweight, she had to be removed from that list, which added to her anxiety. The cystic fibrosis was ravaging her body, and Courtney knew she was not getting better. Her younger brother, Trevor, was regularly carrying her from the bedroom to the bathroom or piloting her around in a wheelchair.
The Eleventh Hour
Such was her condition when Courtney again checked in to St. Paul last August. She was feeling worse than usual, and it became apparent why days later when her other lung collapsed. This time doctors could not reinflate the organ, no matter what they tried. Her condition was dire and getting worse.
“We thought we were losing her,” says Courtney’s mom, Laura, an office manager at a hedge fund company in Dallas. She quickly needed to make decisions. Laura’s bosses offered to fly Courtney to wherever was needed for her to get the best care. “My company knows all about Courtney, and its health care team actually got involved in looking for where the best place to take her would be,” Laura recalls. “After researching it, they said we already were at the best place and that UT Southwestern doctors were innovative. I said, ‘OK, that’s all I need to know.’”
By the first week of October, Courtney was, by all accounts, in her eleventh hour. Carbon dioxide was accumulating to extremely dangerous levels in her blood, and her oxygen levels were very low. A special Short-Term Support team led by J. Michael DiMaio, M.D., Surgical Director of UTSW’s Lung Transplant Program, swung into action and stabilized Courtney using a portable heart-lung machine, the latest advancement in mechanical circulatory support systems. The machine can quickly be connected to a patient in an emergency situation, and without it, her doctors say, Courtney would not have survived.
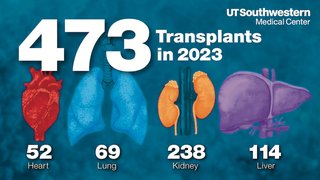
Meanwhile, Dr. DiMaio, together with Fernando Torres, M.D., Medical Director of the Lung Transplant Program, made the decision to perform a double-lung transplant, and Courtney was moved to the top of the transplant list.
A week later, on Oct. 10, donor lungs became available, and Courtney received her transplant. Two weeks later, she was home.
Courtney says she will never forget what it was like to take her first breath after getting new lungs.
“At first I wouldn’t breathe deep because I didn’t think I could,” she says. “It took kind of a retraining of my brain, but once I did, it was like going from breathing through a straw my whole life to suddenly just being able to gulp air and taste it. It was so different.”
‘Miracle Girl’
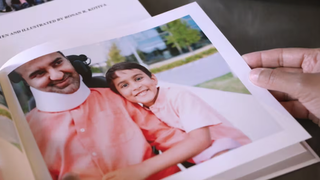
Today, Courtney and her mother say they consider UT Southwestern part of their family. In the months following her transplant, Courtney remained a regular on campus, traveling to St. Paul five days a week — three days for physical therapy and two for clinical appointments. Every time she arrived, the receptionists and nurses greeted her enthusiastically, calling her “Miracle Girl.”
Courtney’s physical therapy ended in January this year, cutting down the number of her visits. But toward the end of February, she suffered a setback. As is the case with 20 percent to 30 percent of cystic fibrosis patients after a transplant, Courtney was diagnosed with diabetes. Her reaction to the news, which according to her mom is entirely characteristic, was, “It could be worse.”
That response did not surprise Dr. Torres, who has come to know Courtney and her family well. “It’s her fight for living — that’s one of her gifts,” Dr. Torres says.
Dr. DiMaio concurs: “The resiliency she has is not something you can read about on her electronic medical record or see on the paper chart — it doesn’t come across there. You have to see people like Courtney and talk to them to realize the energy, the emotion, the fire in the eyes that exists and is what is going to get them through.”
There’s another reason as well, if you ask Courtney’s mom. “She’s the strongest person I know, and she’s always dealt with whatever’s been given to her. But there’s no doubt we wouldn’t have her still here if not for the whole UT Southwestern team,” Laura says.
A Survivor’s Perspective
While Courtney is now more active than ever, her life is more regimented. Twice daily, she checks her blood pressure, temperature, and pulse, measures her lung capacity, and then logs those numbers in a book. She will continue to do that and remain on antirejection medications — part of the more than 35 pills she takes daily — for the rest of her life. In addition, since the diabetes diagnosis, she now has to have insulin shots. The routine seems grueling until one considers it from Courtney’s perspective.
“People all the time say, ‘Oh, it’s so terrible you had to have a transplant,’” she says, “but I say, ‘No, it’s not. It’s good. It’s great! I have my life back — and I can breathe!’”