Fixing trigger finger with a fresh approach
October 24, 2025
When retired orthopedic surgeon Price Burdine developed trigger finger, a frustrating and often painful hand condition, he expected a long road to restore normal function. He tried conservative treatments, including steroid injections. But none of these managed the stiffness, limited range of motion, and incessant snapping and locking in his right ring finger for very long.
“Every time I grabbed my walking stick, the finger would pop," Dr. Burdine said. "Doorknobs or anything that hit the palm, I couldn’t grab it. It was very annoying.”
Then he learned about a new technology and treatment option that uses real-time ultrasound guidance to release trigger finger in the doctor’s office – with no stitches or anesthesia. Dr. Burdine, who performed traditional trigger finger surgery during his career, said the relief was remarkable, and almost immediate.
“Within two weeks, I could confidently grasp or grab anything I needed.”
Jonathan Cheng, M.D., a Professor in the Department of Plastic Surgery who specializes in hand surgery, became the first UT Southwestern surgeon to perform the minimally invasive trigger finger release (TFR) procedure. And he’s been impressed with the results and the lasting benefits for his patients like Dr. Burdine.
“Traditional trigger finger release surgeries are performed in the operating room and require a friend or family member to bring the patient home afterward,” Dr. Cheng said. “This new procedure is done in the office with local anesthesia, takes only about an hour, and they can go on with the rest of their day.”
TFR also has the potential to provide lasting relief from trigger finger’s stubborn symptoms, some of which are not always well-controlled with more traditional surgical methods.
“Minimally invasive TFR spares patients from lengthy downtime,” added Dr. Cheng. “The recovery is easier and shorter, the outcomes are excellent, and since it is an outpatient procedure, there are fewer logistical challenges to getting patients the relief they need quickly.”
What is trigger finger?
There are 27 bones, 34 muscles, and more than 100 ligaments inside a healthy human hand. There is also a system of flexor tendons, or tough cords that attach muscle to bone and help the fingers move. These tendons are surrounded by thick, soft tissue that forms a protective tunnel, through which they slide to move the fingers without stretching too far away from the bones.
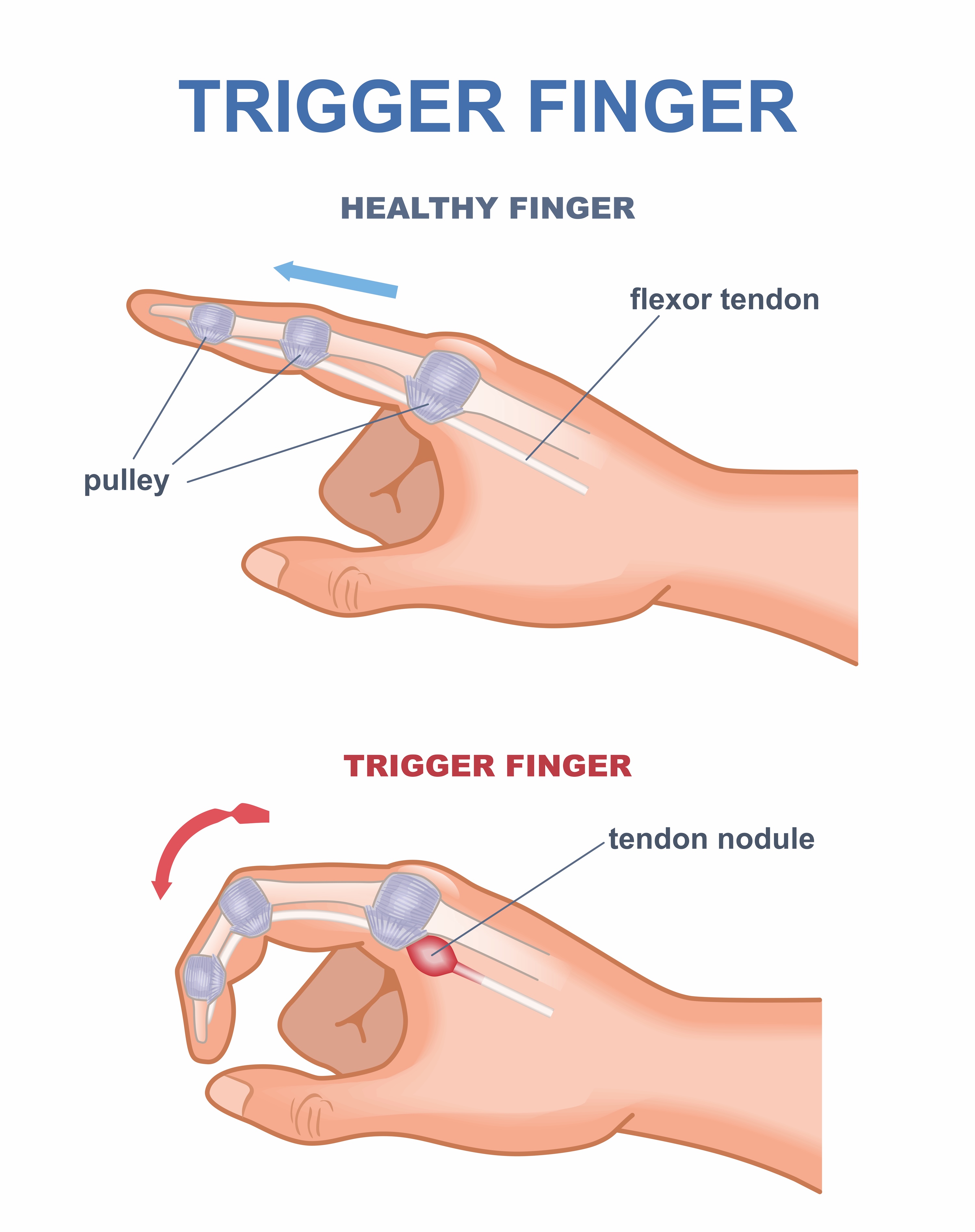
Stenosing tenosynovitis, more commonly known as trigger finger, occurs when a tendon in the finger gets caught in the tunnel due to inflammation or the development of a knot (nodule) on the tissue. This causes disruptive symptoms, which can include:
- Pain or stiffness when moving the finger
- Finger locking in position with a snapping sensation
- Popping or clicking when moving the finger
- Tenderness or a painful bump in the palm at the base of the finger
Trigger finger can develop at any age and can affect a single digit or multiple fingers – most often the ring finger and thumb. Though a cause can’t always be identified, some factors that can increase your risk include:
- A career or hobby that involves repetitive hand motions or prolonged gripping. This can include farming or gardening, working with tools, or playing racket sports such as tennis or pickleball.
- Health conditions such as diabetes or rheumatoid arthritis that involve inflammation.
What are the treatments for trigger finger?
Treatment for trigger finger usually starts with resting the hand as much as possible and avoiding activities that require repetitive gripping or grasping. Other therapies include taking a nonsteroidal anti-inflammatory drug such as ibuprofen, wearing a splint, and doing gentle stretching exercises to help maintain mobility in the finger.
If these options aren’t enough, steroid injections can reduce inflammation in the hand.
“I have patients who have been coming to see me for steroid injections every two or three years, sometimes every six months,” Dr. Cheng said. “Having to come in for repeat injections can interfere with your life.”
Patients who don’t get lasting relief from injections may benefit from surgery to widen narrow portions of the tunnel for better tendon movement. Traditional trigger finger surgery can provide good results, but it involves getting general anesthesia in the operating room and a half-inch incision in the palm that requires stitches and can take several weeks to heal.
Dr. Cheng said that because minimally invasive TFR eliminates many of these challenges, he’s starting to recommend it for patients whose symptoms persist after a few injections.
Related reading: Restoring hand function impaired by Dupuytren’s contracture
What to expect from minimally invasive TFR
After checking in at the clinic, you will get an injection in your hand to numb it. You will be awake during the procedure, but you will not feel anything. Using local anesthesia instead of general anesthesia allows you to communicate with the surgeon during the procedure and avoid feeling groggy afterward.
“We’re accomplishing the same goal as with traditional trigger finger release surgery, but because we use ultrasound guidance, we don’t need to make a large incision to visualize the field. It makes a big difference in recovery time and getting someone back to their normal activities faster.”
Jonathan Cheng, M.D.
When your hand is numb, the surgeon will make a four-millimeter incision (about a quarter inch) in the palm of your hand at the base of the affected finger. Using an ultrasound wand to identify the anatomical structures of the finger and hand, the surgeon will then insert a special device through the incision and into the tunnel surrounding the affected tendon. A tiny blade will be deployed through the TFR device to open the tissue and release the tendon, unlocking the finger to allow for a normal range of motion.
“We’re accomplishing the same goal as with traditional trigger finger release surgery, but because we use ultrasound guidance, we don’t need to make a large incision to visualize the field,” Dr. Cheng said. “It makes a big difference in recovery time and getting someone back to their normal activities faster.”
We will ask you to move your finger in various ways to verify that the problem has been fixed. Once the TFR device is removed, we will close the incision with wound tape or a small bandage. No sutures or stitches are needed.
Most patients, like 56-year-old architect Michael Mamer, find that they can resume regular activities within a week or two.
“I went back to work after I was done with the procedure, and there was no pain because of the local anesthetic,” he said. “It was just a little tough to use a mouse that first day, but I played in a golf tournament three or four days later.”
For patients like Dr. Burdine and Mr. Mamer who grappled with trigger finger symptoms after conservative treatment, getting minimally invasive TFR surgery can be a gamechanger.
“Gripping is easier now, and I have full range of motion in my right hand with no locking or stopping midpoint,” said Mr. Mamer. “If you’re on the fence about getting this procedure, do it!”
Trigger finger affects 2%-3% of the general U.S. population and up to 20% of people with diabetes. It is one of the most common hand conditions treated in the UTSW Department of Plastic Surgery, where our skilled physicians perform hundreds of delicate hand surgeries each year. Adding minimally invasive TFR as a treatment option means our patients will have access to another advanced procedure that can quickly restore function and improve their quality of life.
To talk with an expert about treatment options for trigger finger, make an appointment by calling 214-645-8300 or request an appointment online.











