Novel Drug Combination Fights Resistance to TKI Therapy
October 26, 2020
Clinical Trials at UT Southwestern
As an academic medical center, UT Southwestern offers clinical trials that give eligible patients access to the newest therapies. Learn more about clinical trials at UT Southwestern.
A new drug pairing discovered at the UT Southwestern Simmons Cancer Center might extend the effectiveness of a lung cancer treatment and make it available to many more patients.
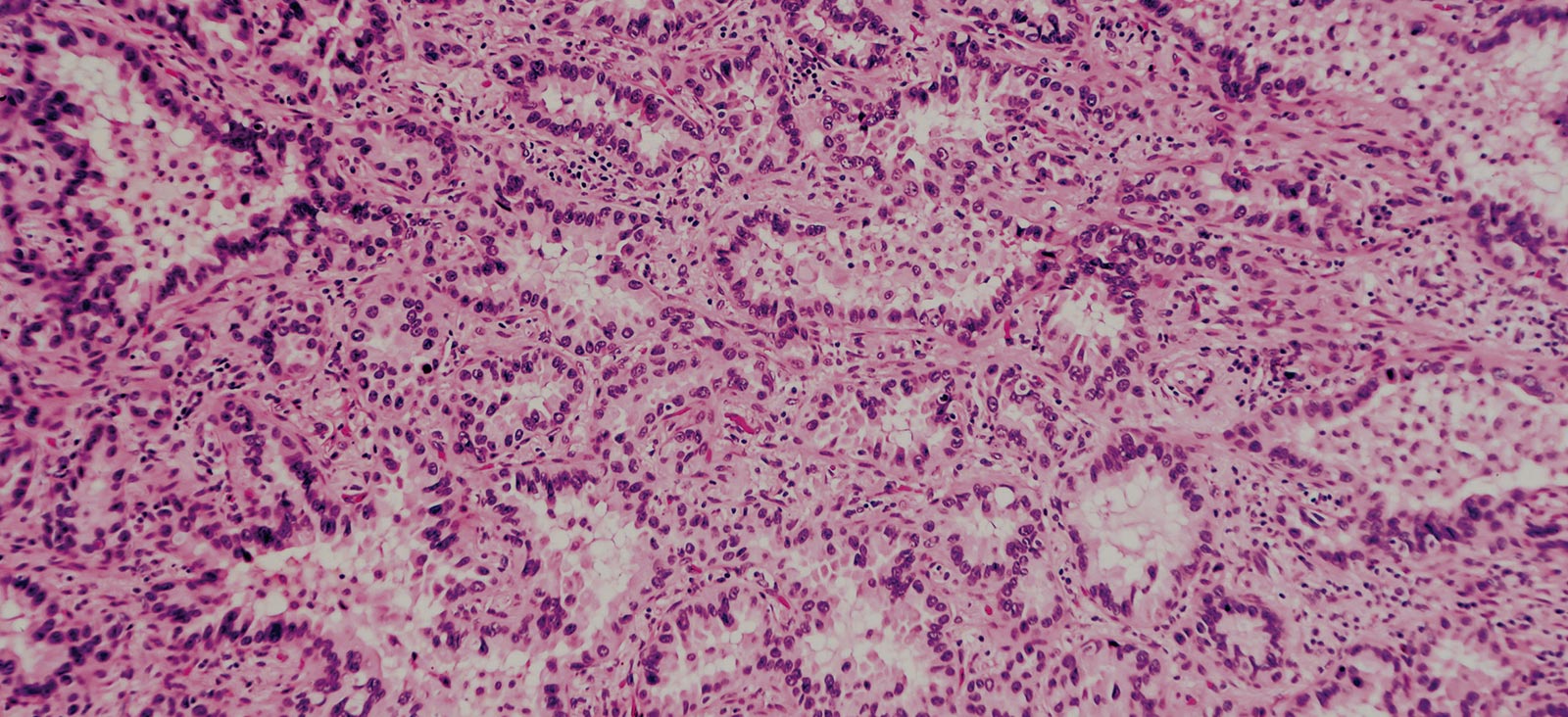
The treatment landscape of non-small cell lung cancer (NSCLC) has significantly advanced over the past two decades due to improved understanding of disease tumor biology, mechanisms of resistance, and earlier diagnosis. The widespread uptake of biomarker-guided targeted therapy has extended survival for patients in the metastatic setting, but continued research into new therapies and combination approaches is needed to broaden clinical benefit and further improve outcomes for patients with advanced lung cancer. [1]
Epidermal growth factor receptor (EGFR) inhibitors have proved to be an effective treatment for patients with EGFR-activating mutations. Since all NSCLC will eventually become resistant to single agent EGFR tyrosine kinase inhibitor (TKI) therapy, one area of ongoing research is how to overcome resistance to TKI therapy. [2-3]
EGFR receptors are frequently expressed or mutated in various forms of cancer. The motivation underlying our current research is to improve treatment for patients with EGFR-mutated NSCLC, and we are actively pursuing clinical trials with a novel combination of EGFR-TKI and IFN-neutralizing antibody.
IFN-I Signaling and EGFR-TKI Sensitivity in NSCLC
Mutations in the EGFR tyrosine kinase are found in about 15% of NSCLC adenocarcinomas in the U.S. and observed more often in nonsmokers. [4] The decision to use an EGFR TKI is based on detection of these mutations using either solid tissue biopsies or liquid biopsies. [5] The underlying molecular mechanisms and signaling pathways contributing to TKI resistance in EGFR-mutant lung cancer are still being elucidated, but recent research has shown that inhibition of mutant EGFR elicits type I interferon (IFN)-I upregulation via an RIG-I-TANK-binding kinase 1 (TBK1)-IRF3 pathway. [2] Furthermore, inhibition of EGFR wild-type (EGFRwt) upregulates IFNs via an NF-κB-dependent pathway. [2]
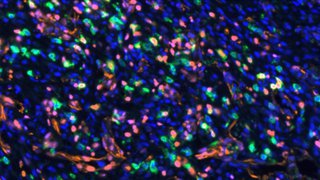
Recent work by our team showed that inhibition of IFN signaling enhances EGFR-TKI sensitivity in EGFR-mutant disease and renders EGFRwt NSCLC sensitive to EGFR inhibition in preclinical models. They also observed that tumors with less IFN-I expression are more sensitive to EGFR-TKI therapy. These results suggest that IFN-I signaling is a central component of EGFR-TKI response and that combination treatment with an EGFR-TKI and IFN-neutralizing antibody might be viable for patients with NSCLC, but further clinical studies are needed to validate these results. [2]
I’m very excited about the results of our current study that was completed in xenograft and immunocompetent animal models. Looking ahead, we hope these findings will translate to the clinic.
“Results suggest that IFN-I signaling is a central component of EGFR-TKI response and that combination treatment with an EGFR-TKI and IFN-neutralizing antibody may be viable for patients with NSCLC.”
Amyn Habib, M.D.
Future Research
Our team at UT Southwestern is actively leading the development of novel therapies for patients with NSCLC. We are working in collaboration with other experts at our institution to develop new and innovative therapies. As one of the nation’s leading academic medical centers, we offer access to pivotal early- and late-stage clinical trials aimed at optimizing outcomes for patients with all stages of lung cancer. In addition, our trials often provide access to breakthrough therapies that are not available elsewhere. [6]
David Gerber, M.D., Professor of Internal Medicine within the Hematology/Oncology Division at UT Southwestern and Co-Director of the Experimental Therapeutics Program, is also investigating novel biomarker-guided targeted therapies for adults with lung cancer. Currently, he and his team at UT Southwestern are enrolling patients into clinical trials evaluating EGFR-targeted treatment in metastatic NSCLC. [7]
In the near future, I would like to test this novel combination in lung cancer patients. Simmons is an exceptionally strong cancer center, and we have several researchers working on many exciting lung cancer clinical trials.
About the Author
Amyn Habib, M.D., Associate Professor in the Department of Neurology and Neurotherapeutics at UT Southwestern Medical Center, is a renowned expert in the treatment of patients with neurological disorders and leads an active research laboratory exploring the biology of EGFR signaling and mechanisms of resistance to EGFR-targeted treatment in glioblastoma and NSCLC.
Footnotes
1. Herbst RS, Morgensztern D, Boshoff C. The biology and management of non-small cell lung cancer. Nature. 2018;553(7689):446-454.
2. Gong K, Guo G, Panchani N, et al. EGFR inhibition triggers an adaptive response by co-opting antiviral signaling pathways in lung cancer. Nat Cancer. 2020;(1):394-409.
3. Gerber DE. EGFR inhibition in the treatment of non-small cell lung cancer. Drug Dev Res. 2008;69(6):359-372.
4. Kawaguchi T, Koh Y, Ando M, et al. Prospective analysis of oncogenic driver mutations and environmental factors: Japan molecular epidemiology for lung cancer study. J Clin Oncol. 2016;34(19):2247-2257.
5. Merker JD, Oxnard GR, Compton C, et al. Circulating tumor DNA analysis in patients with cancer: American Society of Clinical Oncology and College of American Pathologists joint review. J Clin Oncol. 2018;36(16):1631-1641.
6. Utswmed.org. Lung Cancer Clinical Trials. Accessed July 3, 2020.
7. Utswmed.org. David Gerber, M.D. Accessed July 3, 2020.