Many of us have something about our appearance we wish we could change. It might be a scar, bony limbs, or too much weight around the middle. The pressures of beauty and body images all around us – especially on social media – don’t help. Most people can acknowledge their perceived flaw, then go about their day.
Body dysmorphic disorder (BDD) is very different. I often describe this psychiatric condition as a mental trap: a person becomes intensely preoccupied with a specific body feature they see as flawed, asymmetric, or unattractive.
To others, the feature looks normal. To the patient, it is constantly top of mind and overwhelming. The condition is rooted in the brain’s perception systems and may involve serotonin dysregulation, a chemical that plays a role in depression, joy, and a broad range of other neural messages.
Among those with BDD, preoccupation with a perceived flaw can consume hours each day, disrupting school, work, and relationships. Some individuals seek unnecessary cosmetic procedures to try to “fix” the flaw.
These oppressive symptoms typically lead to significant feelings of shame and isolation; BDD has one of the highest suicide attempt rates of any psychiatric disorder. Experts estimate that half of people with BDD experience suicidal thoughts, and about one in four attempt suicide over their lifetime.
BDD is more common than people realize, affecting an estimated 2%-3% of people worldwide.
Despite these factors, BDD often stays hidden. Well-meaning loved ones or even health professionals who are unfamiliar with the condition may invalidate the person’s concern with comments like “You look fine” or “You’re overthinking it.”
BDD is real – many people struggle for years before finally getting the right diagnosis. But once it is identified by experts, such as those at the Peter O'Donnell Jr. Brain Institute at UT Southwestern, the condition is highly treatable. A personalized care plan will put you on the path to feeling better in your own body.
How is body dysmorphic disorder diagnosed?

When we meet with a new patient, we ask questions to determine the extent of their preoccupation. For a diagnosis of body dysmorphic disorder, a patient meets three key criteria:
- Preoccupation with a perceived defect that is minimal or unobservable to others.
- Repetitive behaviors or mental acts related to the concern.
- Clinically significant distress or impairment.
Body dysmorphic disorder is not the same as an eating disorder such as anorexia nervosa or bulimia nervosa. A BDD patient does not drastically change the way they eat or think about food, and they do not have a fear of gaining weight. Instead, someone with BDD develops a fixation on a specific body part or feature, rather than achieving a specific weight or shape.
Symptoms typically begin in the teenage years when social comparison, bullying, and cultural pressure around attractiveness can heighten concerns about appearance. Some patients fixate on a specific feature such as their skin, hair, nose, or jawline. Others focus on body symmetry or signs of aging.
BDD also manifests with repetitive or even ritualistic behaviors such as:
- Checking mirrors or taking numerous selfies, or, conversely, avoiding mirrors and cameras altogether.
- Camouflaging the perceived flaw with makeup, hats, hair, masks, or specific lighting.
- Repeatedly seeking reassurance.
- Excessively grooming or touching the area.

Some of these behaviors may be hidden, such as constant mental comparisons to what they see as “normal” people. People with BDD genuinely believe the flaw makes them fundamentally ugly, worthless, or unlikeable. These thoughts and behaviors can consume hours, disrupting daily life. On average, BDD obsessions and rituals take up three to eight hours a day.
For these individuals, the distress is visceral, regardless of what others see or how much reassurance is given. They may skip activities due to shame and drop out of school or stop working and become housebound; some turn to alcohol or drugs to numb the pain.
Preoccupation with appearance is at the core of BDD. However, because avoidance is a noticeable symptom, BDD is frequently mistaken for depression, social anxiety disorder, or obsessive-compulsive disorder (OCD). About 75% of people with BDD also have major depressive disorder, 40% have a clinically significant social anxiety disorder, and about one-quarter have also been diagnosed with OCD.
What’s happening inside the brain
Research shows that BDD is not a matter of low self-esteem or insecurity. Rather, it is a distortion in how the brain interprets appearance-related information.
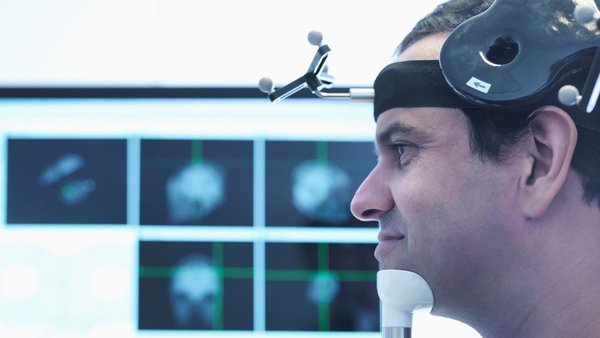
Functional magnetic resonance imaging (fMRI) has shown that the visual occipital cortex, the back part of the brain that deals with vision, behaves differently in people with BDD. Their brains may focus intensely on minute details, demonstrating an enhanced perception of visual detail. They are less able to interpret the “big picture” of their body as a whole, which may explain their increased attention to miniscule features.
Related: Read “Inside the brain of someone with an eating disorder”
What are the treatment options for body dysmorphic disorder?
When we treat BDD in the clinic, we evaluate the severity of the patient’s preoccupation. We also screen for other coexisting conditions such as depression, anxiety, or substance use.
Determining the best approach comes from a shared decision-making process. Some patients prefer to start with therapy; others want medication to reduce their distress enough to engage fully in therapy. With the right mix of therapy and medication, most patients see a significant improvement in their symptoms within 4-16 weeks.

Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is central treatment for body dysmorphic disorder. This proven method focuses on:
- Understanding the disorder
- Identifying distortions in appearance-related thinking
- Reducing checking and avoidance behaviors
- Addressing shame
- Improving insight
- Relearning how to interpret faces and body cues
A key component of CBT is exposure and response prevention. Supported by their care team, patients learn to participate in situations that cause distress without performing self-soothing rituals.
Medication
For patients who choose to take medication, a class of anti-anxiety drugs called selective serotonin reuptake inhibitors (SSRIs) can be very effective. Medications such as fluoxetine (Prozac), sertraline (Zoloft), or paroxetine (Paxil) can reduce the frequency and severity of worries about appearance and repetitive behaviors as well as relieve emotional distress and reduce suicidal ideation. SSRIs are safe and well-tolerated, even at the higher doses needed to help manage BDD.
Following the initial intensive treatment, most patients stay on maintenance medication for two to three years. This allows them to build up an extended period of stability as they put their new coping skills into practice. At that point, we may slowly reduce the dosage if the patient chooses to do so.
TMS: How specialized magnets relieve medication-resistant depression
- Naveed Khokhar, M.D.
August 14, 2025
Why we don’t recommend cosmetic procedures
Experts estimate that up to 40% of people with BDD seek cosmetic surgery. We strongly discourage cosmetic treatment for BDD symptoms because:
- Surgery does not correct the underlying condition
- Dissatisfaction often returns quickly
- Suicidal thoughts may worsen when surgery fails to relieve distress
- The preoccupation may shift to a new area
Studies show that about 14% of patients in cosmetic dermatology settings meet BDD criteria. Experienced plastic surgeons know to screen patients for BDD and will refer them to mental health specialists before offering a procedure. My own interest in this area actually began when a UT Southwestern medical student interested in plastic surgery asked me how to identify patients at risk of poor outcomes. That question sparked years of deeper study.
How to respond to someone with BDD
Many individuals with BDD have told at least one friend or family member about their concerns and have been dismissed. “You look fine” or “stop obsessing” feels invalidating when their brain is sending a very different message.
Instead, it’s better to focus on:
- Listening
- Understanding the burden
- Exploring goals and values
- Reducing shame
- Highlighting that BDD is treatable
You are not alone, and you can feel better
Body dysmorphic disorder is painful, isolating, and often misunderstood. But with the right support, you can rediscover confidence, hope, and the ability to re-engage with the world.
The path to healing starts by asking yourself:
- Are my appearance‑related thoughts or rituals keeping me from my goals at school, at work, or in relationships?
- How much time and energy am I losing to checking, camouflaging, or comparing my appearance or avoiding situations and events?
- Have I pursued cosmetic procedures that didn’t relieve the distress?
If you answered “yes” to any of these, we can help you find the right diagnosis and get effective treatment. Body dysmorphic disorder is a profound challenge, but it is not a life sentence. Don't give up – help is available.
To talk with an expert about body dysmorphic disorder, make an appointment by calling 214-645-8500 or request an appointment online.