Pancreas transplants transform lives for people with severe diabetes
March 31, 2025

Having severe diabetes means constantly having to make decisions to manage it. In fact, research shows some patients make as many as 180 decisions a day about their care: Do I need to take more insulin? Eat a snack? Check my blood sugar? Refill my prescription? That’s on top of every other decision a person makes in a day.
But even if you make all the right choices, diabetes symptoms can still get out of control for some people. More than 30 million U.S. adults have been diagnosed with diabetes, and most patients can control their disease with medication and lifestyle changes. However, some develop significant diabetes-related health problems such as kidney disease, vision loss, nerve damage, or extreme sugar level fluctuations. If this is the case for you, you might be a candidate for a pancreas transplant or kidney-pancreas dual organ transplant.
These lifesaving procedures can:
- Eliminate or significantly reduce the need for insulin, dietary restrictions, and routine blood sugar checks.
- Reverse or lessen the impact of diabetes complications, such as vision changes and kidney dysfunction.
- Prevent organ damage caused by uncontrolled diabetes.
As of September 2024, more than 2,100 people are on the national kidney-pancreas waitlist. The survival rate for patients 10 years after a kidney-pancreas transplant is 70%, which is significantly higher than survivorship for patients with Type 1 diabetes on maintenance dialysis who are on the transplant waiting list.
As the largest transplant program in North Texas, we are dedicated to giving as many people as possible a second chance for not just a longer life but also a much healthier, higher quality one. Our experts here at UT Southwestern understand the profound impact transplant procedures can have on patients, which is why we have established expertise in the medical and surgical management of patients requiring pancreas or kidney-pancreas transplants who have with severe Type 1 diabetes or select Type 2 diabetes with low-functioning insulin production and insulin resistance.
How can a pancreas transplant help me?

One of the main functions of the pancreas is to make insulin, a hormone that helps your body use sugar for energy. Diabetes causes your pancreas to make too little insulin, not use it well, or both – this is why you have to inject insulin to control your blood glucose levels.
Sometimes, taking insulin is not enough, leading to uncontrolled blood sugar levels that can cause damage throughout the body. A pancreas transplant replaces the function-deficient organ with a healthy one that produces an appropriate amount of insulin. In some cases, patients also need a new kidney due to chronic kidney damage from diabetes. A pancreas transplant can help improve – and in some cases reverse – diabetes complications such as:
- Retinopathy: Damage to the blood vessels of the retina in the eye due to uncontrolled high blood sugar levels, which can lead to blindness
- Peripheral neuropathy: Nerve damage that can cause loss of sensation in the feet, increasing the risk of ulcers and infections that can result in amputation
- Gastroparesis: Paralysis of the stomach, a condition in which the stomach empties too slowly, resulting in abdominal pain, nausea, and vomiting
Getting a pancreas transplant can help a woman become healthy enough for pregnancy, with specialized follow-up care and medication adjustments. Over time, controlling high blood sugar can decrease the risk of serious diabetes complications such as blindness, stroke, limb loss, heart disease, and artery diseases.

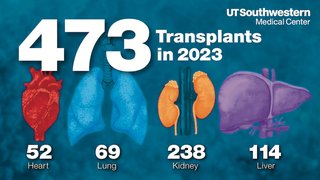
Improving lives with transplants
UTSW recently celebrated its 5,000th transplant procedure. It has remained the largest transplant program in North Texas by volume for the fifth consecutive year, performing 462 transplants in 2024.
Who may qualify for a pancreas transplant?
A pancreas transplant is a major procedure. Our specialists recommend this procedure only for patients who will benefit based on specific criteria. You may qualify for a pancreas or kidney-pancreas transplant if you have:
- Type 1 diabetes that cannot be controlled with standard treatment.
- Type 2 diabetes with both low insulin resistance and low insulin production (less common than Type 1 diabetes-related transplants).
- Kidney damage due to diabetes.
- Hypoglycemic unawareness, meaning you cannot detect when you have a steep drop in blood sugar.
Your specialist team will also evaluate factors such as your age (generally 50 or younger), body mass index, and overall health to determine whether transplant surgery would be safe for you.
Pancreas or kidney-pancreas transplant is not a safe option for patients with pancreatic cancer or kidney cancer. People may not be eligible due to certain conditions, including:
- Blood vessel disease in the leg or neck
- Lung disease
- Hepatitis or other infections
- Substance use, such as illegal drugs, tobacco, or alcohol
The testing for eligibility includes blood tests, urinalysis, diabetes evaluation, heart and lung function tests, and an eye and dental exam. We will also perform a psychological evaluation and examine your hands and feet for loss of sensation.
Related reading: Son gives ‘most meaningful gift’ to father and stepfather
What to expect
Before a pancreas transplant
If you are eligible for and choose to have a transplant, you will be placed on the organ transplant waitlist. At UT Southwestern, the average wait time for a deceased-donor kidney is about two years, compared to the national benchmark of 3-5 years. For a pancreas and kidney together, the average waiting period is a little more than 9 months.

The transplant team will discuss your transplant options based on your health needs and goals:
- Pancreas transplant: This may be done if you have no evidence of kidney disease.
- Kidney-pancreas transplant: Kidney disease is one of the most severe complications of diabetes. You may need this combined surgery if you have or are at risk of kidney failure.
- Pancreas-after-kidney transplant: This often occurs when a person with kidney failure gets a kidney transplant. They are then eligible for a pancreas transplant once they have recovered from the surgery and a pancreas becomes available.
During your waiting period, your care team will support you to remain as healthy as possible. This includes properly treating wounds or ulcers so that they heal, taking your medications as prescribed, quitting tobacco use, eating a healthy diet, limiting alcohol, and staying physically active. We will also help you prepare for surgery and recovery through educational resources during visits, with take-home materials, and in peer support networks.
Once a donor pancreas becomes available, it must be transplanted within 12 hours. People on the waitlist should keep a bag packed and to be ready for travel to the hospital on short notice.
During a pancreas transplant
During the surgery, you will be asleep under general anesthesia. The surgeon will make an incision along your abdomen from above your belly button to your pubic bone. The new pancreas will be placed on the right side of your abdomen and attached to nearby blood vessels and your small intestine. Your own pancreas will be left in place to aid in digestion.
If you are also getting a new kidney, it will be placed on the left side of your abdomen and attached to nearby blood vessels, and the ureter will be connected to the bladder. A kidney-pancreas transplant typically takes four to six hours.
Related reading: Living-Donor Kidney Transplant
After a pancreas transplant
Your recovery will begin in the intensive care unit, where we will monitor your condition for a couple of days and watch for signs of complications. From there, we’ll move you to the surgical ward for about a week of continued recovery and education on the permanent lifestyle changes required for living well with an organ transplant, such as:
- No tobacco or alcohol use
- Eating a healthy diet
- Maintaining a good blood pressure
- Maintaining a proper body weight
- Following your medication plan
For the rest of your life, you will need to take immunosuppressive medication to prevent your body from rejecting the donor organs. Call your doctor right away if you notice signs of infection or organ rejection, such as:
- Fatigue or general discomfort
- Fever
- Chills or body aches (flu-like symptoms)
- Redness, leaking, or tenderness at the incision site
- Decreased urine output
- Nausea or vomiting
- High blood sugar
Pancreas transplants require intensive follow-up care, especially during the first three months after surgery. You will visit with our specialists once a week for a month. If you live more than two hours away, we may ask you to stay in the area for the first month given the frequency of visits and lab draws required. Regular follow-up visits will continue, but at spaced out intervals the further you are from transplant.
You can start to lift light items and do some gentle exercise after about six to eight weeks. Depending on the type of work you do, you may need to take a couple of months off to recover.

Group support available
The Transplant Support Group meets virtually every third Wednesday of the month from noon-1 p.m. The group is for patients and their families to share their experiences about transplants. Led by a social worker, the group provides emotional support and tips for living with a transplant. For more information about the Transplant Support Group, call 214-645-5505.
Thriving after a pancreas transplant
Your new pancreas should start making insulin right away, meaning you’ll no longer need insulin to treat your diabetes. In the rare event your new pancreas doesn’t make enough insulin, it’s likely that you will still be able to control your blood glucose levels more easily with medication than before the surgery.
Getting a pancreas transplant can significantly improve your quality of life. Along with not needing insulin injections, you’ll be able to lead a more normal life with fewer restrictions – and fewer moment-to-moment decisions about managing your health.
Your risk of developing complications associated with diabetes will decline as your freedom from the constant demands of diabetes management increases. And for those decisions you will need to make before and after a pancreas transplant, we’ll be by your side.
To talk with an expert about whether you may be a candidate for pancreas transplant, make an appointment by calling 214-645-8300 or request an appointment online.