Detecting and treating a rare form of gynecologic cancer
September 5, 2025
Quick links: Symptoms | Diagnosis | Treatment | Prevention

For many women, the first symptoms of vulvar cancer are often overlooked or dismissed as a something as innocuous as a heat rash or a reaction to a new hygiene product.
But the truth is that skin changes, bumps, persistent itching, and sores that don’t heal in that “private” part of the body are simply not topics that most women feel comfortable talking about – even with their doctors. That silence, rooted in cultural stigmas surrounding women’s sexuality and genitalia, can cause delays in care for a cancer that is very treatable when caught early. The five-year survival rate for localized forms of vulvar cancer is about 86%.
Vulvar cancer affects about 6,500 women in the U.S. each year, and it can occur at varying stages of life. More than 50% of cases develop in women 70 and older; another 20% involve women under 50. Yet awareness about vulvar cancer remains relatively low. Nearly 60% of women surveyed recently had never heard of it, and 8 in 10 said they had never done a self-exam for early signs or symptoms.
As the only National Cancer Institute-designated comprehensive cancer center in North Texas, UT Southwestern is a high-volume center for the diagnosis and treatment of vulvar cancer at every stage. Our nationally recognized experts and multidisciplinary teams provide patients with access to the most advanced research, clinical trials, and therapies.
By increasing awareness about vulvar cancer – and all gynecologic cancers – we hope women will feel empowered to trust their instincts, overcome the stigma, and talk to their doctors so they can get the compassionate, evidence-based care they deserve.
What is vulvar cancer and what causes it?
Cancer of the vulva, or the external skin and area surrounding the urethra, vagina, clitoris and labia, typically develops slowly over several years.
The exact cause is unknown, but it is often associated with two conditions:
- Human papillomavirus (HPV), a sexually transmitted infection spread through skin-to-skin contact
- Lichen sclerosus, a rare, chronic condition that causes patches of thin, itchy skin to develop primarily on the genitals
There are several varieties of vulvar cancer:
- Squamous cell carcinoma is the most common (about 90% of cases) and is found in the smooth tissue that lines the vulva.
- Melanoma develops in the pigment-producing cells in vulvar skin. It has a high risk of spreading to the lymph nodes and other areas of the body.
- Adenocarcinoma occurs in the fluid-producing cells in the vulvar lining.
- Sarcoma arises in the soft tissue of the vulva.
- Basal cell carcinoma is usually caused by sun exposure. It is a very rare form of vulvar cancer.
Related reading: Demystifying ovarian cancer
What are the symptoms?
Cancer can form anywhere on the vulva, though its first symptoms usually appear on the labia, or outer and inner lips of the vagina.
Symptoms may include:
- An itchy lump or sore that doesn’t heal for a month or more
- Color changes or thickening of the skin
- Pain and tenderness, particularly during sex or urination
- Irregular bleeding (not menstrual)
- A mole that changes size, color, or shape
These symptoms resemble other, less series conditions, which can lead to confusion among patients and even some providers.
Meet Dr. Lea, Chief of Gynecologic Oncology
Board certified in gynecologic oncology and obstetrics and gynecology, Jayanthi Lea, M.D., specializes in the comprehensive care of patients with ovarian, endometrial, cervical, and other gynecologic malignancies.
How is vulvar cancer diagnosed?
The doctor or Ob/Gyn specialist will start by discussing your health history and conducting a pelvic exam to inspect the vulva, vagina, and cervix, looking for unusual skin changes. They may use a lighted, magnification tool called a colposcope to provide clearer views and a special solution to highlight abnormal cells.
While HPV tests and regular Pap smears can help spot early signs of cervical cancer, they are not able to detect vaginal or vulvar cancers. The only definitive way to diagnose vulvar cancer is with a biopsy, which involves removing a small sample of the tissue to test it in a pathology lab for cancer cells.
Vulvar cancer often produces visible or physical symptoms, however, so while there is no specific screening for it you should consider conducting regular self-exams.
If vulvar cancer is confirmed by a biopsy, additional imaging tests will help determine the stage of the cancer.
- Stage I: The cancer is confined to the vulva or the perineum, which is the area between the vulva and the anus.
- Stage II: It has spread to nearby tissues but not lymph nodes.
- Stage III: Cancer has spread to lymph nodes or adjacent areas.
- Stage IV: It has spread to other parts of the body.
Related reading: How cervical cancer screening with HPV testing is saving lives
How is it treated?
Surgery is the cornerstone of vulvar cancer treatment.
As a large academic medical center, UT Southwestern has extensive experience treating vulvar cancer at every stage. Early-stage vulvar cancers can be cured with surgery alone. Our gynecologic oncologists are experts at individualizing surgery and vulvar reconstruction. When cancer is contained to the vulva, the goal is to remove the tumor and enough surrounding tissue to effectively cure the cancer. In select situations, we may also perform a sentinel node biopsy, removing the lymph node(s) closest to the tumor to determine whether the cancer has spread to the groin. If those nodes are cancer-free, we can avoid a full lymph node dissection (lymphadenectomy).
For patients who require additional treatment, our gynecologic oncologists work closely with colleagues from Radiation Oncology to provide patients with precise external-beam radiation to eliminate the tumor entirely.
In more advanced cases, external beam radiation therapies can be used to shrink the size of their tumors prior to surgery. Chemotherapy may be recommended along with radiation to reduce the size of the tumor before surgery.
Vulvar cancer and gynecological tumors in general are often located near critical tissue, including the bladder, rectum, ovaries, and reproductive/sexual tissues. Because of the proximity to these normal healthy tissues, UT Southwestern often uses radiation to precisely target a tumor while also sparing healthy tissue and reducing side effects.
Related reading: The ART and science of targeting gynecologic tumors
Preventing and reducing vulvar cancer risk
About half of all vulvar cancers are caused by HPV infections, which are very common and usually don’t lead to cancer. The HPV vaccine was approved by the Food and Drug Administration (FDA) in 2006, and it has significantly reduced the threat of cancer-causing HPV. It is most effective when given to patients before they become sexually active. It can also be obtained by women up to age 45, but it is less protective in older ages.
Some other risk factors for vulvar cancer include:
- Smoking tobacco
- Skin conditions such as Lichen sclerosis
In addition to scheduling regular check-ups, including pelvic exams, women should use a mirror to regularly examine their vulva for any changes. Pair it with your monthly self-breast exams as a valuable way to safeguard your health. If you notice or experience any symptoms, please see a doctor right away.
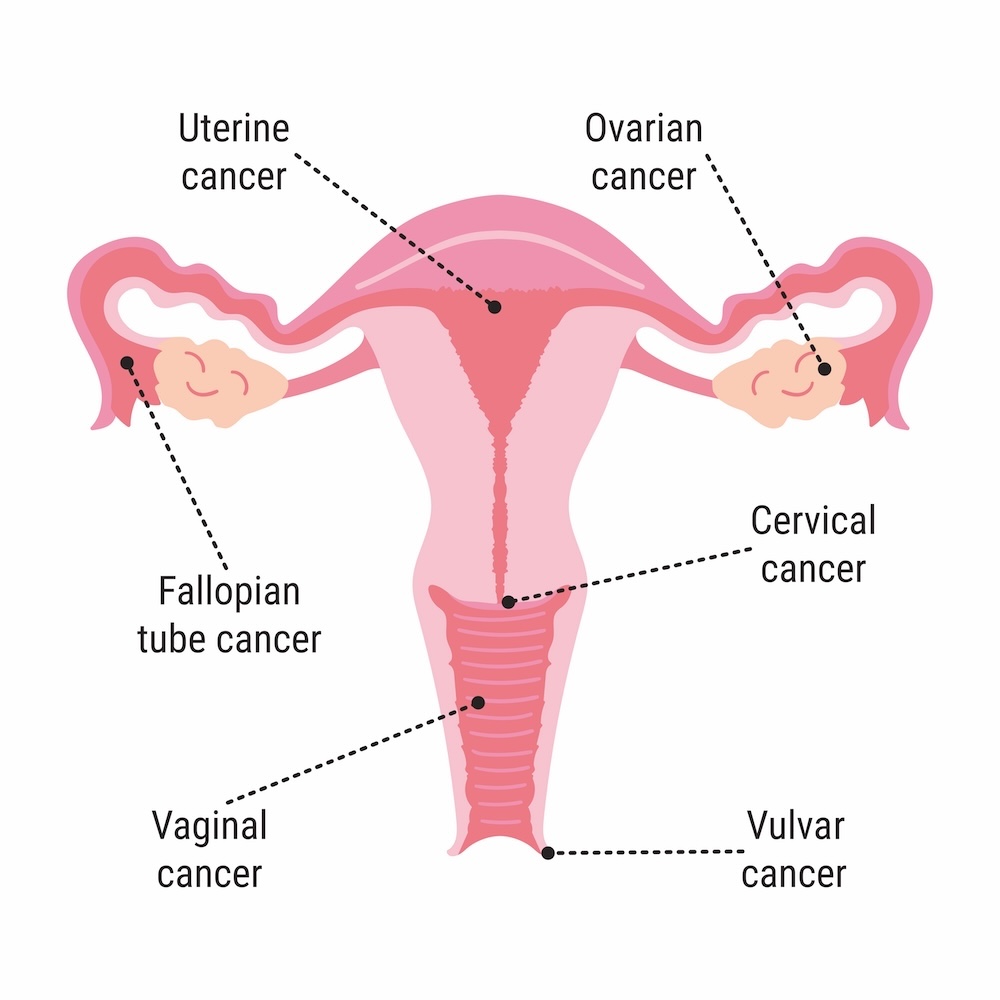
Every September, Gynecologic Cancer Awareness Month focuses on educating the public about the five main gynecologic cancers affecting the female reproductive system: cervical, ovarian, uterine/endometrial, vaginal, and vulvar cancers.
The common theme across all gynecologic cancer is that early detection is key. Silence is never the best option. At UT Southwestern, we understand that you may feel uncomfortable asking certain questions regarding gynecologic cancers or raising concerns about how treatments could affect sexual function and fertility.
Our experts are here to answer all of your questions, treat you with respect and compassion, and provide you with the best care possible. To talk with a specialist from our gynecologic oncology team, make an appointment by calling 214-645-3838 or request an appointment online.











