Case Study: Novel Pola-RICE Drug Protocol for Stage 4 Lymphoma
January 20, 2026

A Simmons Cancer Center team created a collaborative, multistage treatment plan that put a 22-year-old’s cancer into remission.
Unless you work directly with lymphoma patients, you may not know that lymphoma is an umbrella term for more than 80 unique cancers that form in lymphocytes. These cells can reside in the approximately 600 lymph nodes, liver, and spleen that comprise the immune system. Lymphoma tumor cells are found in these tissues, in the bloodstream, and in the bone marrow where healthy blood cells are normally formed.
Lymphoma can cause vague symptoms such as swollen lymph nodes, fever, weight loss, and persistent coughing or chest pain. As a result, approximately 33% of people with non-Hodgkin lymphoma have stage 4 disease upon diagnosis.
There is no standard treatment protocol for lymphoid malignancies, particularly for drug-resistant lymphomas. Each subtype and each patient responds differently to medical and radiation oncology approaches.
Therefore, effective treatment requires a multidisciplinary team that intentionally unites its members’ clinical expertise, research, and technology to manage each case.
The only National Cancer Institute-designated Comprehensive Cancer Center in North Texas, the UT Southwestern Harold C. Simmons Comprehensive Cancer Center is ranked in the top 20 for cancer by U.S. News & World Report, which also recognizes the treatment of leukemia, lymphoma, and myeloma as “high performing,” placing UT Southwestern among the nation’s top institutions for this area of care.
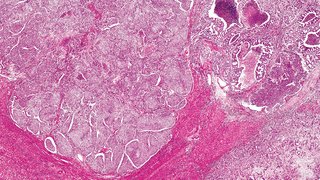
This case study shows the positive effects of multidisciplinary lymphoma care. A 22- year-old male patient with stage 4 large B-cell lymphoma was referred to the Simmons Cancer Center after treatment options at two previous centers were exhausted. His chest and abdomen were crowded with tumors. Previous chemotherapy and CAR T-cell therapy cycles were ineffective.
Farrukh Awan, M.D., M.S., M.B.A., Professor of Internal Medicine at UT Southwestern and a member of the Division of Hematology and Oncology, created a collaborative, multistage, nine-month treatment plan that put patient Erik Torres’ two-year cancer ordeal into remission. Today, Torres has no evidence of detectable cancer cells in his body.
"Effective treatment of lymphoma requires a multidisciplinary team that intentionally unites its members’ clinical expertise, research, and technology."
Pola-RICE: Combined Antibody Therapy and Chemotherapy
Spring 2024: Torres enrolled in a Simmons Cancer Center clinical trial of epcoritamab, a bispecific T-cell engager antibody medication; Torres’ cancer did not respond. However, the next treatment protocol would prove successful.
Torres completed two cycles of polatuzumab vedotin with rituximab (Pola-R), a combination of synthetic monoclonal antibodies. The antibodies homed in on two specific cancer cell surface antigens and activated the immune system to eliminate the cancer cells. As a result, Torres experienced significant tumor shrinkage and improved blood counts.
On the third cycle, Dr. Awan added three chemotherapy drugs — ifosfamide, carboplatin, and etoposide — to create the novel combination Pola-RICE. Within three cycles of Pola-RICE, repeat imaging was negative for malignancies. Using highly sensitive cancer detection technology that can find one cancer cell among a million normal cells, the team concluded there was no evidence of circulating cancer cells.
Total Marrow Lymphoid Irradiation (TMLI)
Spring 2024: Torres began TMLI, an advanced radiation therapy technique that, along with chemotherapy, conditioned Torres’ immune system prior to an allogeneic stem cell transplant. Radiation oncologists as well as experts in stem cell transplantation and nuclear medicine mapped Torres’ anatomy and tumor sites, then modulated and programmed radiation beams to precise areas of Torres’ body.
Team-based coordinated care is paramount for successful TMLI, which can require weekly 48-hour hospital stays, ongoing modulation, and close communication among inpatient and outpatient providers. UT Southwestern is one of a handful of centers in the United States with the infrastructure and clinical expertise to offer TMLI.
Allogeneic Stem Cell Transplant
Summer 2024: Torres received an allogeneic stem cell transplant in an inpatient infusion procedure, which is comparable to getting dialysis. During recovery, he developed graft-versus-host disease (GVHD), which can occur after any type of transplant. GVHD can be life-threatening if severe or inappropriately managed.
Julio Alvarenga Thiebaud, M.D., Assistant Professor of Internal Medicine at UT Southwestern, is an expert in managing GVHD and de-escalating the risk of further complications. Over a six-week hospital stay, Torres received immune suppression therapy and palliative treatment for GVHD-associated nausea, diarrhea, and musculoskeletal pain.
Fall 2024: Torres made a full recovery and transitioned home to continue healing. By December 2024, he was feeling like himself again. As of late 2025, imaging and blood assays showed that he remains cancer-free.
Collaboration Key to Successful Lymphoma Care
Expertise and collaboration are key to successfully managing exceptional cancer cases like the one described here. As an NCI-designated Comprehensive Cancer Center, the Simmons Cancer Center takes on even the most complex cancers, either referred by other oncologists in the region or when patients find us on their own.
Every patient’s case is reviewed by our multidisciplinary lymphoma board, which includes internationally recognized research leaders, pathologists, radiation oncologists, medical hematologist-oncologists, imaging specialists, advanced practice providers, and specialized nurses. These experts provide insights from every angle to create effective, customized, and integrative treatment plans.
Positive outcomes like the one with this patient would not be possible under the care of a single physician. Through intentional collaboration, we develop technological advancements; clinical trial opportunities; and new, effective treatments that continually improve patients’ health.

About the Experts
Farrukh Awan, M.D., M.S., M.B.A.
Professor, Internal Medicine, Division of Hematology and Oncology Member, Experimental Therapeutics Research Program, Harold C. Simmons Comprehensive Cancer Center

Julio Alvarenga Thiebaud, M.D.
Assistant Professor, Internal Medicine, Division of Hematology and Oncology