Expanding Eligibility Criteria for Cancer Clinical Trials
July 20, 2020
Clinical Trials at UT Southwestern
As an academic medical center, UT Southwestern offers clinical trials that give eligible patients access to the newest therapies. Learn more about clinical trials at UT Southwestern.
Many studies are now more inclusive, thanks to the work of experts at UT Southwestern.
Clinical trials in the U.S. struggle to enroll patients. Fewer than 5% of adults with cancer in the U.S. enroll in clinical trials, and a substantial proportion of clinical trials close before they finish because they are unable to meet accrual targets or, because it takes so long to meet the accrual numbers, the study is no longer relevant. [1,2] On top of that, a general criticism of clinical trials is that their eligibility criteria are so selective that the results are not generalizable to real-world patients.
Under this pretext, I grew increasingly frustrated that a number of my patients who came to see me for lung cancer clinical trials were not eligible because they had a history of an earlier cancer, and this often was the only reason they were ineligible. The referring physicians shared this frustration, and it was especially so for the patients because they didn’t understand why a prior cancer should prevent them from participating in a study.
I began to wonder: (1) How common is this practice? (2) How does this practice affect enrollment in clinical trials? and (3) Is this practice justified? In other words, what proportion of lung cancer clinical trials exclude patients with a prior cancer? How common is a prior cancer diagnosis among patients with lung cancer? And do lung cancer patients who had an earlier cancer have worse outcomes than patients who did not have a prior cancer?
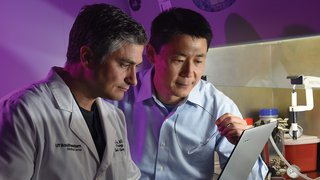
These questions led me to reach out to other experts, including health outcomes expert Ethan Halm, M.D., M.P.H., Professor of Internal Medicine and Population and Data Sciences, epidemiologist Sandi Pruitt, Ph.D., Associate Professor of Population and Data Sciences, and statistician Lei Xuan, Ph.D.
Exclusion Factors
Initially, we reviewed a set of 51 National Cancer Institute (NCI)-sponsored lung cancer clinical trials (total enrollment 13,072) and found that 80% of them excluded patients who had a prior cancer. [3] Among trials that had a primary endpoint of survival, 94% excluded patients with a prior cancer. Even among trials with nonsurvival primary endpoints, such as measures of biomarkers, feasibility, or safety, 73% excluded patients with a prior cancer.
Next, we examined the prevalence and prognostic impact of a prior cancer diagnosis among more than 200,000 patients with lung cancer in the SEER (Surveillance, Epidemiology, and End Results) database of the NCI. Among patients with early-stage lung cancer, 24% had an earlier cancer [4]; similarly, 15% and 16% of patients with locally advanced or metastatic lung cancer, respectively, had a prior cancer. [3,5] When we applied these data to the individual lung cancer trials we reviewed, we estimated that up to 18% of potential patients would be excluded solely because of a prior cancer, which translated to more than 200 excluded patients in large phase 3 trials.
“The NCI has stopped excluding patients with a prior cancer from lung cancer clinical trials. These studies are improving the way we think about, design, and implement clinical research.”
David Gerber, M.D.
Importantly, the majority of prior cancers were within five years of the lung cancer diagnosis, were early-stage tumors, and were frequently highly treatable malignancies, such as prostate or bladder cancer.
Lastly, we compared the clinical outcomes of lung cancer patients with and without a prior cancer diagnosis. This analysis revealed that having a prior cancer was never associated with worse all-cause or lung cancer-specific survival, regardless of the type, timing, and stage of the prior cancer. [4,5]
Based on this work, the NCI has stopped excluding patients with a prior cancer from lung cancer clinical trials. Many pharmaceutical companies have done the same. These studies are improving the way we think about, design, and implement clinical research. This work is relevant not only to lung cancer but to any type of cancer and, arguably, to any type of clinical research.
About the Author
David Gerber, M.D., is a faculty member within the Hematology Oncology Division at UT Southwestern Medical Center. At the Harold C. Simmons Comprehensive Cancer Center at UT Southwestern, he serves as Associate Director for Clinical Research and as Co-Leader of the Experimental Therapeutics Program.
Footnotes
1. Lara PN, Higdon R, Lim N, et al. Prospective evaluation of cancer clinical trial accrual patterns: Identifying potential barriers to enrollment. J Clin Oncol. 2001;19(6):1728-1733. doi:10.1200/JCO.2001.19.6.1728
2. Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials. JAMA. 2004;291(22):2720. doi:10.1001/jama.291.22.2720
3. Gerber DE, Laccetti AL, Xuan L, Halm EA, Pruitt SL. Impact of prior cancer on eligibility for lung cancer clinical trials. JNCI J Natl Cancer Inst. 2014;106(11). doi:10.1093/jnci/dju302
4. Pruitt SL, Laccetti AL, Xuan L, Halm EA, Gerber DE. Revisiting a longstanding clinical trial exclusion criterion: impact of prior cancer in early-stage lung cancer. Br J Cancer. 2017;116(6):717-725. doi:10.1038/bjc.2017.27
5. Laccetti AL, Pruitt SL, Xuan L, Halm EA, Gerber DE. Effect of prior cancer on outcomes in advanced lung cancer: Implications for clinical trial eligibility and accrual. JNCI J Natl Cancer Inst. 2015;107(4). doi:10.1093/jnci/djv002