Targeting Phosphatidylserine to Boost Immunotherapy Activity
February 5, 2025
Adding antibody-based therapeutics shows promise in the treatment of hepatocellular carcinoma.
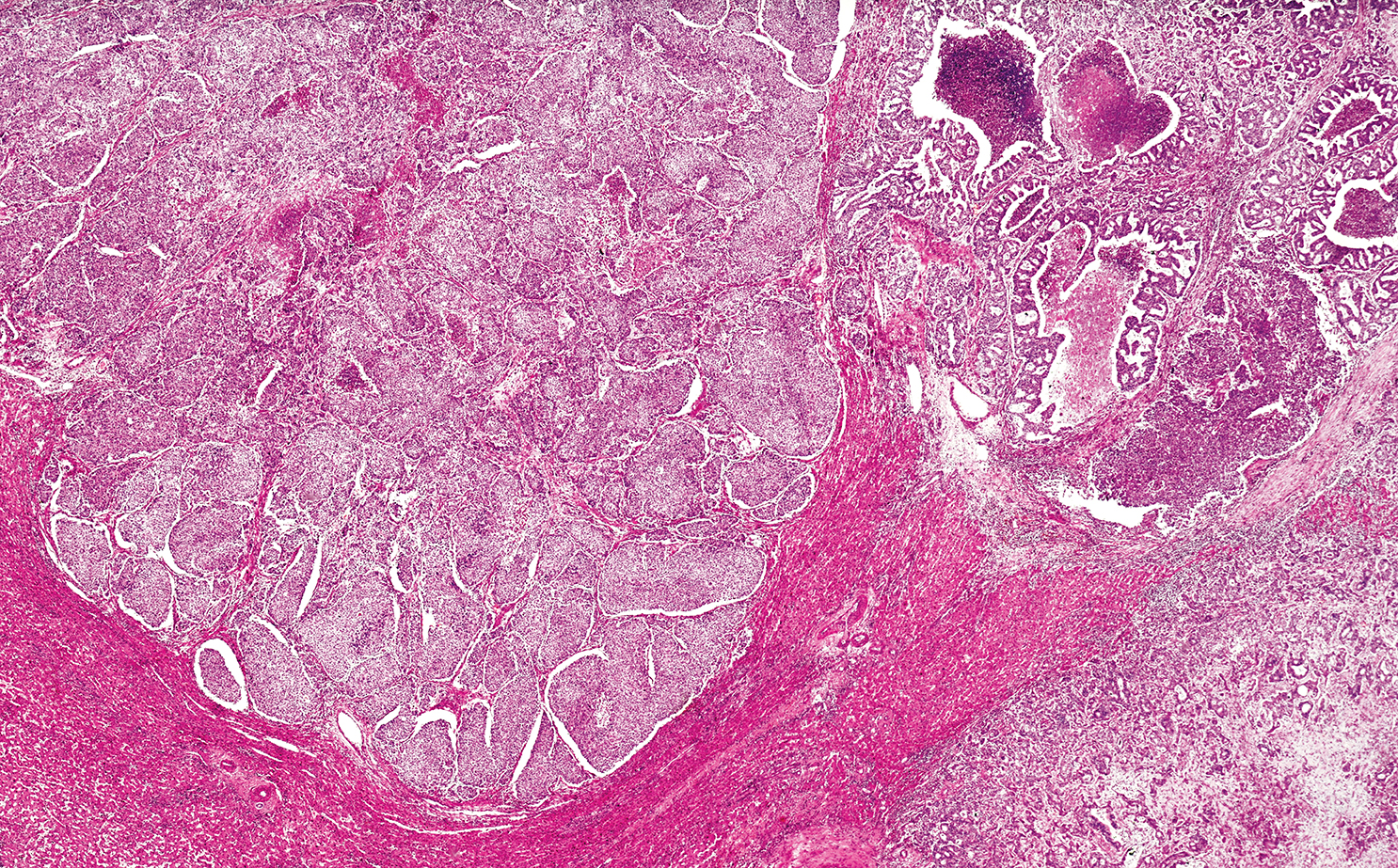
Researchers at UT Southwestern Harold C. Simmons Comprehensive Cancer Center are investigating whether treatments for hepatocellular carcinoma (HCC) can be improved by combining existing immunotherapies with a drug that targets a cytoplasmic-facing anionic phospholipid called phosphatidylserine.
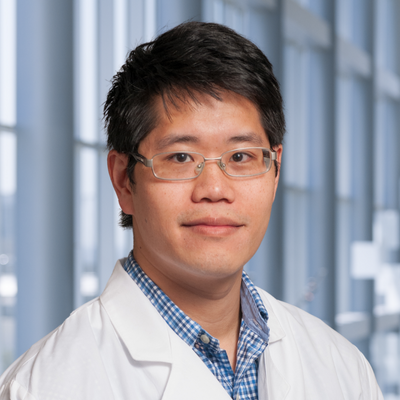
New research published in Nature Communications by David Hsieh, M.D., Assistant Professor of Internal Medicine in the Division of Hematology and Oncology, reveals that the phosphatidylserine-targeting antibody bavituximab may boost the effects of existing immunotherapies without increasing side effects often seen with other drug combinations.
“We hypothesized that targeting phosphatidylserine may be an effective strategy to enhance immunotherapy activity in HCC and other tumors,” Dr. Hsieh says. “The diverse pro-inflammatory and -immune stimulating effects of bavituximab on tumor cells, immune cells, or stroma point toward possible synergy with immune checkpoint inhibitors.”
“These studies are likely to reveal more mechanistic insights.”
David Hsieh, M.D.
Clinical Trial Shows Promise
Dr. Hsieh and his team tested their hypothesis in a single-arm, phase two trial that evaluated the efficacy and safety of frontline bavituximab plus pembrolizumab in patients with unresectable HCC.
Among 35 patients enrolled in the study, 28 were evaluable for the primary analysis. The investigator-assessed objective response rate (ORR) was 32.1%; the median progression-free survival (PFS) was 6.3 months.
With respect to safety, treatment-related adverse events of any grade occurred in 46% of patients, with grade 3 or greater adverse events in only 14% of patients.
“The ORR was similar to that of other dual immunotherapy approaches in HCC,” Dr. Hsieh says. “The response rate of the combo might be due to genuine synergy but warrants confirmation.”
Insights From Correlative Studies
The researchers also explored pretreatment characteristics of the tumor microenvironment (TME) that might play a role in modulating antitumor immunity.
According to Dr. Hsieh, infiltrating B cells have been associated with tumor response in certain solid tumors treated with immune checkpoint inhibitors. These data suggest that B cells may be implicated in mechanisms of cancer rejection.
In contrast to prior research, researchers found that cancers that responded positively to bavituximab and pembrolizumab were linked to low CD20 expression among immune cells. The results indicate that bavituximab could be effective even in tumors with a low B cell presence.
“Due to the widespread expression of phosphatidylserine and its receptors in active immune cells within the TME, bavituximab has the potential to trigger immune responses that involve multiple immune cell types,” Dr. Hsieh adds.
Next Steps
While these findings are encouraging, additional research is needed to better understand the role of anti-phosphatidylserine agents in combination with immunotherapies over existing treatment regimens. Dr. Hsieh notes that the future clinical development plans for bavituximab and pembrolizumab in HCC are being discussed, but correlative studies are ongoing.
“These studies are likely to reveal more mechanistic insights,” Dr. Hsieh says.
David Hsieh, M.D., is Assistant Professor of Internal Medicine in the Division of Hematology and Oncology and a member of the Experimental Therapeutics Research Program at Simmons Cancer Center. He specializes in the treatment of hepatocellular carcinoma, cholangiocarcinomas, and gall bladder cancers and leads clinical trials to test new drugs or drug combinations in these cancers.