The Consequences of Understaging Gastric Cancer
April 30, 2021
Clinical Trials at UT Southwestern
As an academic medical center, UT Southwestern offers clinical trials that give eligible patients access to the newest therapies. Learn more about clinical trials at UT Southwestern.
Patients with nonspecific symptoms that overlap with the symptoms of gastric cancers should be evaluated at a center with extensive experience in treating these cancers.
Treating gastric cancer is a complicated task. The overall incidence of gastric cancer in the United States has dramatically decreased over the last several decades. This declining incidence is due largely in part to improvements in diagnosis and treatment of H. Pylori infection, one of the leading causes of gastric cancer. [1] However, there has also been an unintended consequence of this success — the expertise for efficiently diagnosing gastric cancer has also decreased.
People with gastric cancer often have non-specific symptoms, including weight loss, bleeding, abdominal pain, and acid reflux. Healthcare providers often fail to suspect gastric cancer and treat these symptoms as uncomplicated gastroesophageal reflux disease. As a result, patients with gastric cancer can often face delays in cancer diagnosis. Clinical staging for gastric cancer relies on multiple imaging tests, endoscopic procedures, and sometimes even laparoscopy. Ordering the appropriate staging work up and correct interpretation of the results by providers is necessary for accurate determination of clinical stage. Accurate clinical staging is critical for treatment selection and prognostication.
Low Cancer Incidence May Lead to Inaccurate Staging
As physicians and researchers, we have observed that patients were often understaged prior to starting treatment at UT Southwestern Simmons Comprehensive Cancer Center. We hypothesized that because of the low incidence of gastric cancers in the U.S., the ability to accurately stage these cancers is decreasing. In addition to assessing staging accuracy, we wanted to understand factors associated with inaccurate clinical staging, the impact of inaccurate clinical staging on patient outcomes, and effect of adjuvant therapy in patients with inaccurate clinical staging. [2]
“Increased likelihood of inaccurate clinical staging was associated with clinical stage T2 tumors, non-well differentiated tumors, and diffuse-type histology.”
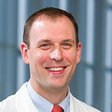
Matthew Porembka, M.D.
We conducted a retrospective review of patients who went straight to surgery for their presumed early-stage gastric cancer, or cancer which has not spread outside of the stomach (AJCC 8th edition; cT1-2, N0, M0), in the National Cancer Database diagnosed between 2004-2016. We classified patients into 3 groups: accurately staged if pathologic staging confirmed early-stage cancer, inaccurately staged with receipt of adjuvant therapy, and inaccurately staged with no receipt of adjuvant therapy.
We found approximately 40% of patients (1675/4244 ) were understaged, having more disease than expected, and we found that many patients had disease in the lymph nodes or even metastatic disease. Increased likelihood of inaccurate clinical staging was associated with clinical stage T2 tumors (which have invaded the stomach muscle layer), non-well differentiated tumors, and diffuse-type histology.
The implications of this inaccurate clinical staging are significant. The standard of care for patients who have regional disease that has spread to the lymph nodes is a combination of chemotherapy and surgery to reduce the risk of cancer recurrence. Treatment begins with the chemotherapy, which is important because it treats any micrometastatic disease that may be present. People who have chemotherapy before surgery tolerate the chemotherapy better. For patients who go to surgery first and have lymph node disease, as many of the patients in our study did, that opportunity to control micrometastatic disease is missed.
Factors Associated with Understaging
Of patients who were inaccurately staged, only 54% received adjuvant therapy, which is guideline-concordant care, and may be associated with overall survival. The 5-year overall survival was significantly higher in patients with accurate staging than in either of the inaccurately staged groups (70% accurately staged, 45% inaccurately staged with receipt of adjuvant therapy, and 40% inaccurately staged with no receipt of adjuvant therapy; p<.0001).
When being treated for gastric cancer, treatment facility type also mattered. Patients treated at academic or integrated cancer network centers were less likely to be inaccurately staged than those treated in the community setting. Additionally, inaccurately staged patients were more likely to receive appropriate neoadjuvant therapy after being clinically understaged at these facilities compared with community facilities. Thus, the implication would be that if a patient has one of these rarer cancers, they should be seen at a center with substantial experience treating patients with gastric cancers to ensure accurate staging and optimal treatment.
In summary, at a national level, we observed inadequate clinical staging of gastric cancers. As a result, opportunities for appropriate treatment are being missed, and understaging is negatively affecting patient survival outcomes. Therefore, we recommend that patients with nonspecific symptoms that overlap with the symptoms of gastric cancers should be evaluated at a center with extensive experience in treating these cancers.
To gain more insight into adequate clinical staging, we are now studying the barriers to care experienced by patients who are evaluated at our clinic. For example, it is common for patients to visit their primary care physician or an emergency department multiple times with complaints of non-specific symptoms. We want to know which specific barriers prevented them from having a gastric cancer workup and earlier treatment. These finding will potentially help us design novel strategies to improve patient care and ensure prompt clinical staging.
About the Author
Matthew Porembka, M.D. is an Associate Professor of Surgical Oncology in the Department of Surgery at UT Southwestern Medical Center. He treats patients with liver, pancreas, stomach, and bile duct cancers at Parkland Memorial Hospital. At Parkland, he also serves as Chief of Surgical Oncology, as Medical Director of Surgery Oncology Clinics, and as Assistant Chief of Surgery.
Footnotes
1. Wang Z, Graham DY, Khan A, et al. Incidence of gastric cancer in the USA during 1999 to 2013: A 50-state analysis. Int J Epidemiol. 2018;47(3):966-975. doi:10.1093/ije/dyy055
2. Ju M, Karalis J, Blackwell J, et al. Inaccurate clinical stage is common for gastric adenocarcinoma and is associated with undertreatment and worse outcomes. JNCI J Natl Cancer Inst. 2020. doi:https://doi.org/10.1245/s10434-020-09403-8