Seeing the big picture: What to expect during a glaucoma evaluation
February 11, 2026
Eyesight depends on a complex web of tissues, fluids, and nerves that move signals from the outside world to our brains, which generate images. Behind the scenes of this production, a common and serious array of eye diseases called glaucoma can creep up over time and threaten your vision.
“Glaucoma” is an umbrella term for a group of eye conditions that damage the optic nerve – the vital connection between your eye and your brain. In a healthy eye, fluid drains away systematically to maintain stable pressure. But in patients with glaucoma, the drainage system is impaired. Pressure rises inside the eye and damages its sensitive nerve fibers, affecting vision.
Glaucoma-related vision loss typically starts with your peripheral vision, which is the outside edges of your sight. It slowly moves toward the central vision field – the area we use for reading, driving, and recognizing faces. The brain is remarkably good at filling in small gaps in our peripheral vision, so many patients don't realize something is wrong until central vision loss begins.
Once glaucoma damage occurs, it cannot be reversed. But the good news is that it is very treatable when caught early.
Today’s technology also allows us to detect subtle changes earlier and more comfortably than ever before. With regular eye exams, timely glaucoma testing, and a care plan tailored to your needs, it’s often possible to slow the disease significantly and preserve vision for decades.
If you’ve been referred for a glaucoma evaluation, or if you’re wondering whether you should be tested, here’s what to know about how glaucoma affects the eye, what happens during an ophthalmology visit, and why ongoing screening is so important.
What are the symptoms of glaucoma?
Often, there are no highly noticeable signs of glaucoma in the early stages of the disease. This is why glaucoma has been called the "silent thief of sight." At your regular eye exams, the optometrist or ophthalmologist may ask if you have noticed any of these symptoms of glaucoma:
- Slow loss of peripheral (side) vision
- Sudden, severe pain in one eye
- Reduced or cloudy vision
- Nausea or vomiting
- Halos around lights
- Redness or swelling of the eye
- Sensitivity to light
- Cloudy appearance in the front of the eye
Sometimes patients worry that acknowledging these symptoms will affect their independence at home or with driving. While we can’t reverse glaucoma, we do have effective treatment options to help preserve your remaining vision and keep the disease from progressing.
Who is at risk for glaucoma?
There are two main types of glaucoma, each with different risk factors:
- Open-angle glaucoma: This is the most common form, where the drainage angle remains open, but the fluid doesn't flow out as efficiently as it should. It typically progresses gradually.
- Angle-closure glaucoma: This occurs when the drainage angle is blocked, which can lead to a sudden, painful rise in eye pressure. This type of glaucoma is a medical emergency and requires immediate treatment to prevent blindness.

Some risk factors for glaucoma include:
- Family history of glaucoma
- Age over 60
- African, Asian, or Hispanic descent
- Defect in the eye at birth
- Extreme nearsightedness or farsightedness
- Thin corneas
- Previous eye injury
- Chronic use of steroid medications
- Diabetes
If you have any of these risk factors or notice changes in your peripheral or central vision, talk with your eye doctor. They may refer you to an ophthalmologist for additional testing beyond your regular eye screenings to help preserve your eyesight.
Related: Read “New glaucoma therapies improve results and reduce recovery time”
How often should you get a routine eye exam?
Even if you have never had vision problems, it’s important to get routine eye exams. The American Academy of Ophthalmology recommends having an eye examination every:
- 5 to 10 years before age 40
- 2 to 4 years for people 40-54
- 1 to 3 years for people 55-64
- 1 to 2 years for people 65 and older
- 1 to 2 years for those who have glaucoma risk factors
People with vision problems, those who wear glasses or contacts, and those with conditions that may affect their eye health, such as diabetes, should consider getting eye exams more frequently.
What to expect at your ophthalmology appointment
There isn’t much you need to do to prepare for a routine glaucoma screening. If you have dry eyes, use over-the-counter artificial tears in the days leading up to your appointment. This optimizes the eye surface, ensuring we get the clearest possible images and the most accurate visual field results. If you have been previously evaluated for glaucoma or another eye condition, it is helpful to bring a copy of any records for your ophthalmologist to review.
Glaucoma evaluations are thorough but generally comfortable and much less intimidating than people expect. In years past, patients sometimes dreaded the "air puff" test in which a quick blow of air on the eye gauged its resistance to pressure. We are happy to share that the UT Southwestern Department of Ophthalmology utilizes a variety of different equipment, including modern and advanced optical screening technology, to comfortably and accurately assess eye pressure and other eye parameters related to glaucoma. These are a few of the exams and measurements you can expect. Some may be done during your initial visit, and depending on your individual case, some may be scheduled during subsequent visits.
Eye pressure measurements
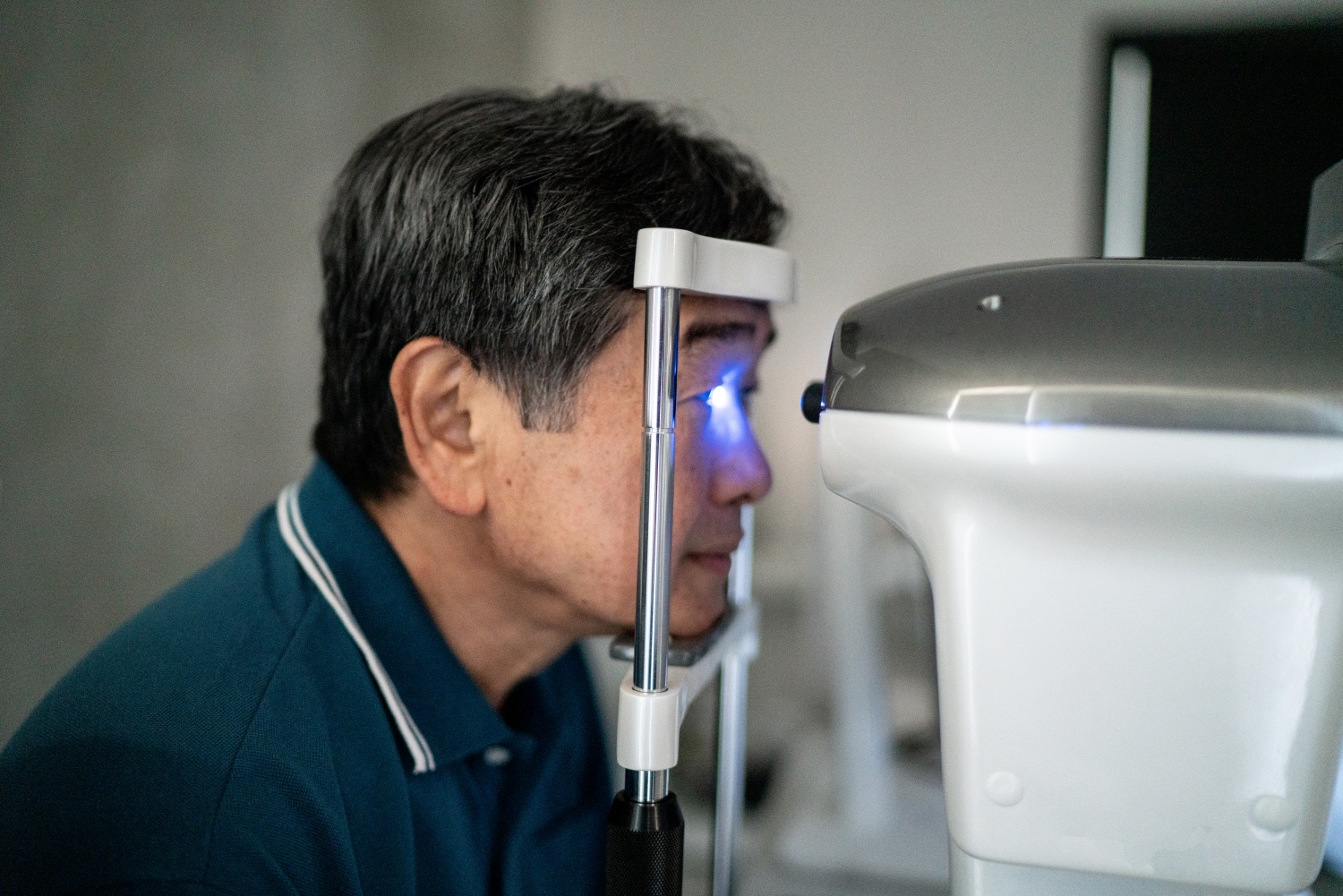
Instead of the eye puff test, we’ll measure your eye pressure with a blue light on an examination microscope. After your eyes are numbed with drops, the device comes closer for a quick, gentle touch on the eye’s surface. This exam is more comfortable than the old method and provides more accurate results.
Visual field testing
The visual field test is one of the most important tools in glaucoma care because it tells us how well you see across your full field of vision. This test helps us:
- Identify "blind spots" that fit the pattern of glaucoma
- Determine how advanced any eye damage may be
- Monitor whether existing glaucoma is stable or progressing
During this test, you’ll sit in front of a domed screen, focusing on a central light with one eye. Small lights flicker in different areas of your peripheral vision, and you’ll press a button whenever you see one. Some lights are bright and easy to spot; others are faint, and you may not be certain you saw them. The test is subjective, and it’s completely normal to miss some of the lights. The goal is to map your vision and catch changes early. This test is regularly repeated to monitor stability versus progression.
Newer technology even allows some patients to complete visual field testing using a virtual reality headset, which can be especially helpful for those with mobility or positioning challenges.
Optical coherence tomography (OCT) nerve scan
OCT is a non-invasive imaging technique that’s similar to an ultrasound for the eye, but it uses light waves instead of sound. The scan provides detailed, cross-sectional images of the retina and optic nerve. It measures the thickness of the nerve fiber layer, helping us detect early signs of glaucoma before vision loss occurs.
You’ll simply look at a target while the machine scans your eye. No eye contact is required, and the test takes mere seconds. We’ll compare your results over time to monitor disease progression.
Color photographs of the optic nerve
Taking high-resolution color images of the optic nerve gives us a valuable baseline for disease progression. With photos, we can compare the appearance of the nerve over months or years to detect subtle changes that could harm your vision.
Central corneal thickness measurement
We measure eye pressure through the cornea, which is the clear front window of the eye, and its thickness can influence the result. We use a handheld device to measure your corneal thickness, which helps us interpret your pressure numbers more accurately. This is a quick, painless screening.
Gonioscopy
Gonioscopy is a specialized exam where a doctor uses a special lens to look directly at the eye’s internal structure to see whether the drainage angle is open or closed. This test is crucial for distinguishing between open-angle and angle-closure glaucoma and guiding treatment decisions.
How we diagnose and treat glaucoma
When we diagnose glaucoma, we aren’t just looking at one number. We look at the results from all the specialized tests: how the nerve looks, how it functions, and how the pressure changes.
Regular eye exams and ophthalmology visits are key to detecting and managing glaucoma. Routine exams with your regular eye doctor catch changes in central vision and eye pressure, while glaucoma specialists perform a more specialized assessment to monitor disease progression and can adjust your treatment plan. This “double coverage” increases the chances of catching glaucoma early and preventing vision loss.
While glaucoma cannot be cured, lowering eye pressure can slow its progression. UTSW ophthalmologists are internationally recognized for our expertise in glaucoma management. Using advanced medications and surgical approaches, we can create precise, customized treatment plans to help preserve your vision and improve your long-term outcomes.
Topical medications
Prescription eye drops are a cornerstone of treatment to reduce intraocular pressure. Most drops pose few, if any, systemic side effects. However, you must use them as prescribed to prevent potentially damaging eye pressure fluctuations.
Selective laser trabeculoplasty
Selective laser trabeculoplasty (SLT) is a gentle laser procedure that helps lower pressure inside the eye by improving how fluid drains out. SLT can reduce eye pressure by about 20%-30%. An ophthalmologist may use SLT as the first treatment before starting glaucoma medication or as the next step if medicines do not fully manage the disease. The procedure is also a good option for people who need or want an alternative to eye drops.
Minimally invasive glaucoma surgery

Minimally invasive glaucoma surgery (MIGS) is a group of newer, safer procedures that help lower eye pressure by improving how fluid drains out of the eye. Some MIGS can be done on their own, while others are performed at the same time as cataract surgery – especially for people with both cataracts and mild to moderate glaucoma.
MIGS surgeries use tiny incisions and cause very little tissue damage, so recovery is usually quicker and safer than with traditional glaucoma surgery.
Traditional eye surgery
For more advanced cases of glaucoma, surgeons can create a new drainage path for the eye fluid:
- Trabeculectomy: This approach uses the eye’s own tissue to bypass the natural drainage system in the eye.
- Tube shunt: This is a flexible drainage tube implanted into the eye to divert fluid inside the eye to an external reservoir.
Surgical pharmaceuticals
UT Southwestern offers what is called bimatoprost intracameral implant (Durysta). This new type of treatment slowly releases pressure-lowering medication into the eye over time. This means you don’t have to worry about remembering to use daily eye drops. A small pellet containing the medication is gently injected into the front part of your eye. The pain-free pellet dissolves on its own and can keep your eye pressure down for several months without the need for drops.
Related: Read “Microinvasive glaucoma surgery, or MIGS, offers reduced risks”
Glaucoma doesn’t announce itself with early symptoms, but its effects can be life-altering. If you have risk factors or a family history, talk to your eye doctor about getting screened. With regular screenings and expert care, we can catch glaucoma early and stop it from progressing, helping you retain your vision and quality of life.
To talk with an expert about glaucoma or other vision concerns, make an appointment by calling 214-645-2020 or request an appointment online.












