How plasma exchange helped save her heart, decades after strep attacked her brain
February 18, 2026
In 1988, when Sherri Merchant was 12, a strep throat infection changed the course of her life.
The Streptococcal virus caused an autoimmune attack on the right side of Sherri’s brain, a cascade of complications now known as post-streptococcal disorders. Sherri was temporarily paralyzed on her left side and had to relearn everyday functions such as walking and writing.
Over time, the after-effects of the strep infection rippled through nearly every system in her body. She developed epilepsy, lupus, kidney disease, and a heart murmur, as well as an exceedingly rare blood clotting disorder.
Ever the optimist, as an adult Sherri faced every new challenge with a smile on her face and her husband, Jonathan, and beloved pets by her side – including a pig named Dobby. The Arlington resident’s greatest joy continued to be serving her special education students at Jo Kelly School in Fort Worth.
In December 2022, Sherri faced her biggest challenge. She had developed persistent bleeding that caused intense abdominal pain, fainting, and severe anemia. Doctors at a local hospital discovered she had lost 5 liters of blood – almost the total amount in the average human body.
They also found a new infection in her heart, which had damaged her mitral valve so significantly that she would need open-heart surgery to replace the valve and to survive. The mitral valve controls the flow of blood from the heart’s left atrium to the left ventricle.
Sherri’s clotting disorder made surgery risky in a community hospital. And without surgery, her outlook was just as grim.
But this time, luck would be on her side.
Sherri’s community doctor was a former medical student of UT Southwestern coagulation disorders expert Yu-Min Shen, M.D. Sherri was referred to UT Southwestern, the only Dallas-Fort Worth medical center with the multispecialty expertise to handle her complex case.
Rare blood disorder, customized treatment pathway

Dr. Shen was the first to connect the dots between Sherri’s persistent bleeding and her lack of clotting factor. Sherri had lupus anticoagulant hypoprothrombinemia syndrome (LAHPS), an autoimmune condition – and hers was only the second case he’d seen in his career.
LAHPS causes problems with bleeding and clotting and low levels of the protein prothrombin due to an anti-prothrombin antibody. While LAHPS is treatable, there is currently no cure.
Dr. Shen reached out to UT Southwestern cardiovascular surgeon Christopher Heid, M.D., who fondly remembers meeting Sherri for the first time.
“She seemed too young, functional, and healthy to not give every effort at finding a way forward,” Dr. Heid said. “The valve surgery wasn’t the complicated part. The challenge was navigating her nuanced medical conditions to get her safely to and through surgery.”
The physicians were determined to find a way for Sherri to have her lifesaving heart valve surgery. The key would be a highly specialized, four-phased procedure before surgery to clear the way for healthy – albeit temporary – blood clotting function.
Plasma exchange: Temporary ticket to clotting
The harmful antibodies associated with LAHPS circulate entirely within the bloodstream. Dr. Shen proposed that to eliminate the antibodies, they’d have to fully replace Sherri’s plasma – the liquid part of the blood – with healthy donor plasma.
Dr. Shen designed a customized therapeutic plasma exchange (plasmapheresis) protocol to temporarily clear Sherri’s destructive antibodies. Each of the four plasmapheresis sessions required several hours of lying flat, connected to tubing that cycled her blood through specialized equipment.
While plasma exchange is not a new or uncommon procedure, using it to help with Sherri’s case was unique. Though the antibodies would return after surgery, plasmapheresis offered a provisional pathway to surgery.
“The idea was to temporarily remove the autoimmune antibody so her prothrombin levels could rise to a safe range,” Dr. Shen said. “In her case, it worked extremely well.”
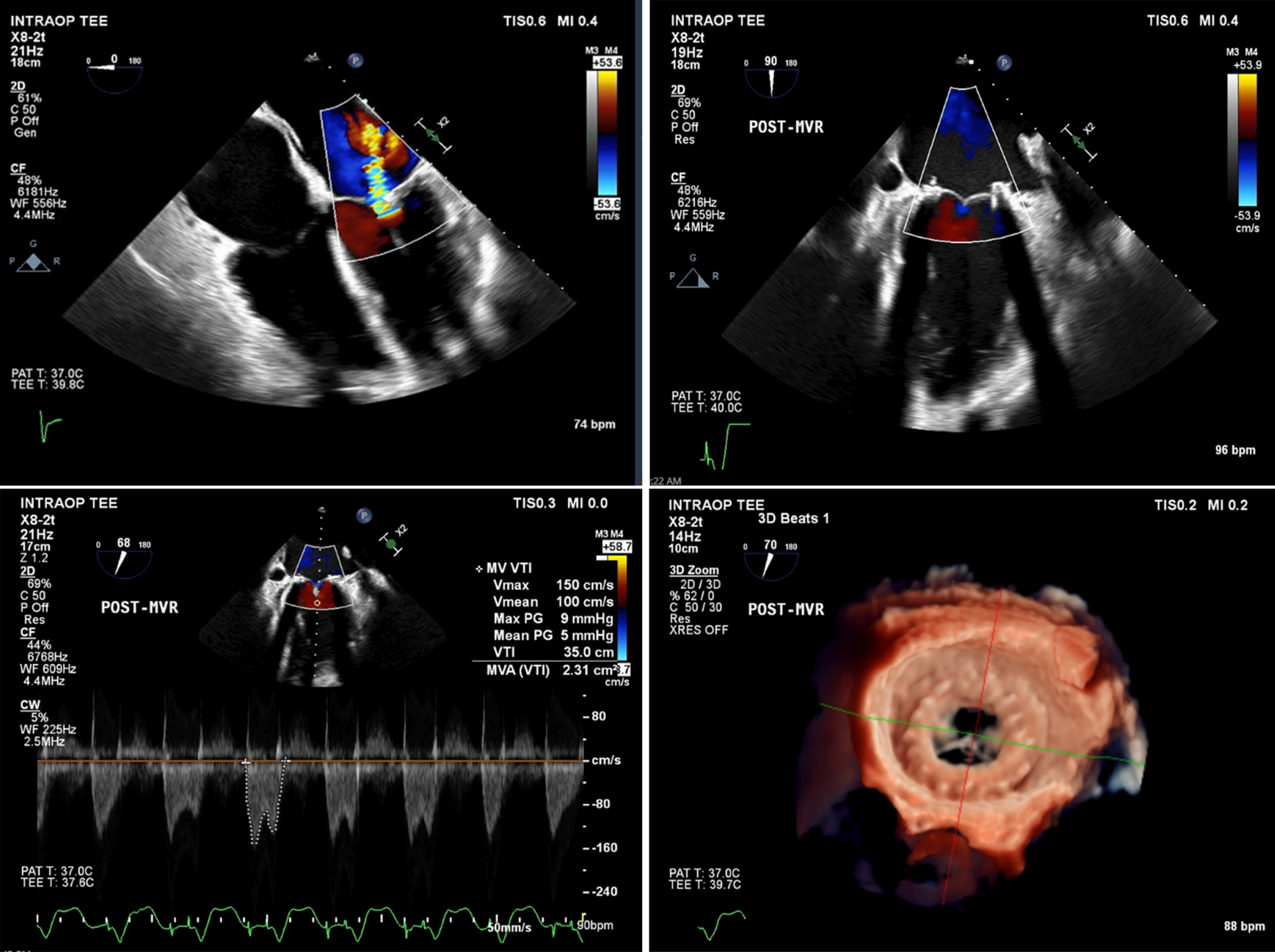
Clockwise from top left: An echocardiogram before Sherri Merchant’s surgery shows mitral valve regurgitation (leaking); a 2D image after surgery shows her newly functioning mitral valve; a 3D reconstruction of the new valve; and an image with color flow measuring the blood flow and gradient across the new valve.
Open-heart valve replacement surgery
On the day of Sherri’s mitral valve replacement in September 2023, her prothrombin levels were high enough to proceed. But not without another twist: Her platelet counts dropped unexpectedly just before surgery. The team adjusted in real time, transfusing platelets into her blood and carefully weighing the risks of going through with the surgery.

“If we couldn’t do surgery, her long-term outlook was very poor,” Dr. Heid said. “The multidisciplinary team agreed that this was our window to save her life.”
Prior to the mitral valve replacement surgery, Dr. Heid consulted with UT Southwestern interventional cardiologist Anthony Bavry, M.D., about surgical options, such as a transcatheter approach, which doesn’t require opening the chest. However, both Dr. Bavry and Dr. Heid agreed that a transcatheter approach was not an option due to the history of endocarditis, or infection of the valve.
Ultimately, Dr. Heid performed open-heart surgery to replace the faulty mitral valve with a bioprosthetic one, which is derived from animal tissues – a fact Sherri loves to point out while snuggling Dobby the Pig.
Why team-based care matters
While Dr. Heid and Dr. Shen led the way on Sherri’s care, her story is a powerful example of how centers like UT Southwestern serve patients with complex, rare conditions.
“We have world-leading experts in every field readily available,” Dr. Heid said. “That multidisciplinary approach – cardiac surgery, hematology, transfusion medicine, anesthesia, and ICU – is essential.”
“They would sit down beside me, not stand at the end of the bed with a clipboard. I felt like I had a friend, not just a doctor.”
Sherri Merchant
Experts from multiple disciplines meet regularly to discuss special cases like Sherri’s. They contributed insights, shaping her care plan while training the next generation of doctors in collaborative problem-solving.
Her case was so unique that the care team, with her permission, has shared her story with other physicians in hopes of helping more patients. Dr. Heid has published a case study, and Dr. Shen has presented her treatment plan at the Great Plains Region of the National Hemophilia Program Coordinating Center.
For Sherri, that teamwork translated into something deeply personal: being treated not as a diagnosis, but as a person.
“They talked with me, not at me,” she said. “They would sit down beside me, not stand at the end of the bed with a clipboard. I felt like I had a friend, not just a doctor.”

Back in the classroom
Before surgery, Sherri could barely walk down the school hallways without help. She had even considered medical retirement. But today, Sherri is back where she belongs, teaching high school students with complex medical needs. Students whose resilience mirrors her own.
“When I went through all this, I didn't know if I was going to be able to teach again,” Sherri said. “My students are a joy to work with.”
As she turns 50 in February 2026, Sherri’s heart is functioning normally. Plasma exchange only temporarily removes the autoimmune antibody that causes Sherri to have low prothrombin levels. Since the inability to clot returned after surgery, she takes an immunosuppressive medication to help maintain her prothrombin levels and sees Dr. Shen for ongoing management.
“Her prothrombin level has decreased modestly since the surgery, but not to the level where she was before,” Dr. Shen said. “And she hasn’t had any trouble since with bleeding. We’ve been pleasantly surprised by that.”
Sherri said each day in her classroom feels like a gift made possible by a team that refused to accept “nothing we can do” as an answer. “I thank God every day for opening that door,” Sherri said. “And for the people at UT Southwestern who walked through it with me.”
To talk with an expert about heart valve repair or replacement, make an appointment by calling 214-645-7700 or request an appointment online.