Transverse myelitis: When inflammation damages the spinal cord ‘wiring’
January 26, 2023

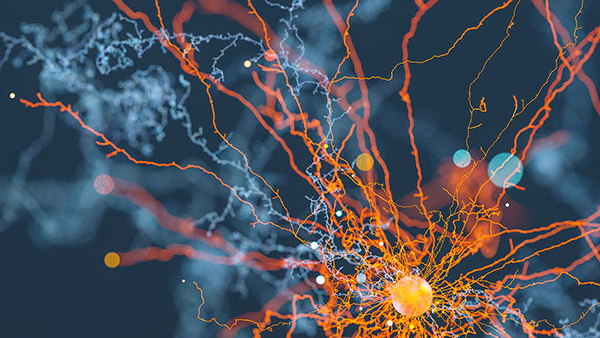
Every day, your body’s internal wiring – an intricate system of neurons and their connections – transmits millions of signals from the brain, through the spinal cord, and into your muscles. Those electrochemical messages control every movement you make.
For example, just to wiggle your big toe, a signal from the brain must travel the length of your body:
- It originates with the upper motor neuron, a “wire” that projects from the brain to the spinal cord, coursing through the white matter area of the brain, and influences muscle control.
- Then the signal is passed along to the lower motor neuron in the gray matter at the center of the spinal cord.
- Lower motor neurons project from the spinal cord to the muscle, inducing movement, telling your toe to flex.
Any inflammation, or swelling, along that pathway can interrupt the brain’s communication with the body – sometimes with devastating consequences.
In a rare condition called transverse myelitis (TM), the body’s immune system mistakes healthy cells in the spinal cord and cause damage to myelin, a tissue sheath that insulates your nerves similar to the insulation on stereo speaker wires. The body mounts an immune response, resulting in inflammation that damages the myelin surrounding the spinal cord. The effects can range from numbness in the limbs or abdomen and balance problems to partial or total loss of the ability to walk, move, see, or control the bowels and bladder.
TM strikes fast – progressing from subtle symptoms to paralysis within weeks, days, or even hours. Making an accurate diagnosis and delivering treatment quickly is critical.
As one of just two dedicated transverse myelitis programs in the world, UT Southwestern has served as an epicenter of research, discovery, and highly specialized patient care since 2009. Along with seeing patients in Dallas – from 47 states and 10 countries, to date – we regularly consult with clinicians around the world to cast a wider net of advanced TM care.
Aggressive, early treatment and focused rehabilitation from our team of specialists are yielding dramatic results, preserving and in some cases restoring sensation and mobility for our patients.
Causes of transverse myelitis
Only a few thousand new cases of transverse myelitis are diagnosed each year in the U.S., but they fall into two categories: secondary or idiopathic (primary) myelitis.
Secondary myelitis is when the cause of spinal inflammation can be identified. A viral infection, such as enterovirus, is an example. Neurological and autoimmune diseases, some of which were only recently defined, can also cause TM.
Multiple sclerosis (MS), is the most common cause of TM. About 25% of MS patients experience spinal inflammation as their first symptom.
Sarcoidosis, an autoimmune disease that causes inflammation in the lungs, skin, eyes, lymph nodes, and liver, can also lead to TM. When the nervous system is affected, it’s called neurosarcoidosis.
Additional recognized types of secondary myelitis include:
- Neuromyelitis optica spectrum disorder, in which the body’s immune system mistakenly attacks specific cells of the spinal cord and eye nerves. This condition was associated with anti-AQP4 antibodies in 2004, and about 99% of patients are adults ages 35-40.
- Anti-MOG associated disorder (MOGAD), in which the immune system attacks the myelin oligodendrocyte glycoprotein on the surface of the outer sheath that covers central nervous system cells. This condition was better defined in 2016 after improvements were made to the blood test commonly used for diagnosis.
- Acute flaccid myelitis (AFM) occurs almost exclusively in children, with 99% of cases in patients younger than 18. AFM progresses quickly and aggressively – in a matter of hours after the first symptom is noticed, a child could experience paralysis. AFM can be caused by viruses that damage motor neurons in the gray matter of the brain.
Idiopathic myelitis is when no clear cause for spinal inflammation can be identified. It can develop in any patient of any age or general health status – my youngest patients have their first symptoms as infants and my oldest in their 80s.
The most likely cause of idiopathic TM is an immune response to a virus the body has cleared and is no longer detectable. The immune system sometimes stays activated after an illness and can mistakenly attack the “wiring” in the spinal cord, causing TM.
Idiopathic TM may also be caused by underlying neuroimmune conditions that have not yet been defined.
'Transverse myelitis strikes fast – progressing from subtle symptoms to paralysis within weeks, days, or even hours. Making an accurate diagnosis and delivering treatment quickly is critical.'
Identifying transverse myelitis symptoms
TM symptoms vary depending on how much damage has been done to specific neurons and areas of the spinal cord. Many symptoms mimic those of MS, but any patient can have a combination of symptoms, which may include one or more of the following:
- Balance disorders
- Bladder or bowel incontinence or retention
- Changes in gait, walking, and muscle coordination
- Numbness or tingling in the waist, chest, or extremities
- Pain
- Sexual dysfunction
- Spasticity
- Weakness
TM develops quickly, distinguishing it from conditions with similar symptoms. In most types of TM, symptom development occurs over two to four weeks. If symptoms are still evolving after four weeks, myelitis is unlikely to be the cause.
AFM can occur literally overnight; I’ve seen children go from healthy and mobile to fully paralyzed within six hours.
Seek help at the first signs of lost sensation. Though most primary care and emergency room doctors are not spine experts, they will be able recognize that the spinal cord “wiring” isn’t working – a situation called myelopathy – and involve a specialist to find out why.
How we diagnose TM
The first step in detecting TM is to confirm via an MRI whether a patient has inflammation of the spinal cord or whether symptoms are coming from a compressive lesion, which means that a disk, tumor, or blood clot is pressing against the spinal cord.
Spinal cord compression is a surgical emergency. Left untreated, it can cause irreversible nerve damage, spinal bleeding, reduced blood flow, and long-term deficits.
If compression is not the cause, we take blood and spinal fluid samples to determine whether the immune system is causing inflammation. We look for specific T-cells, B-cells, and proteins that tell us if the immune system is attacking an infection – or healthy cells – in the spinal cord.
Based on lab work, symptoms, and imaging, we can confirm or rule out a diagnosis of secondary or idiopathic myelitis.TM treatment options
With swift and specialized treatment, there is often significant improvement in symptoms. Recovery from TM can take several months to years and requires a team of experts who can personalize a care plan for each patient’s situation.

Steroids and plasmapheresis
Combining high doses of steroids with plasmapheresis (therapeutic plasma exchange, or TPE) can be extremely effective in potentially curbing damage to the spinal cord.
High doses of steroid medications such as dexamethasone or methylprednisolone are given through an IV, but can be oral, over a few days, to reduce swelling in the spinal cord. TPE involves removing some of the patient’s blood through a large IV and spinning it in a centrifuge to remove specific proteins involved in inflammation. Then, the “clean” blood is returned to the body.
TPE has dramatically improved care in patients, including children. Before our program launched, few children were receiving plasma therapy because it was considered experimental for TM at the time. We pushed the envelope – the more aggressive we got with treatment, the more patient outcomes improved.
Today, many more pediatric patients with TM get TPE. Kids who couldn’t move their legs due to TM are now walking.
Immune suppression therapy
In some patients, suppressing the immune response can stop or slow inflammation enough to contain or halt spinal cord damage.
Patients with neuromyelitis optica, for example, may benefit from medications more commonly used to treat some cancers, autoimmune conditions such as rheumatoid arthritis, Crohn’s disease, lupus; or help prevent organ rejection in patients who have had transplants.
Taking immunosuppressant medication can potentially help prevent future flare-ups if a patient is in a category that requires prevention strategy.
Nerve surgery
In some cases, nerve damage from inflammation can be reversed or improved with specialized surgery. UT Southwestern is a center of excellence for several types of nerve procedures.
For example, Jonathan Cheng, M.D., Professor in the Department of Plastic Surgery, is an expert in nerve transfer surgery, a microsurgical procedure to identify a damaged nerve and replace it with a healthy one from another area of the body. In some cases, the nerve will adapt to its new location and grow, restoring partial or total sensation and function.
Identifying surgical candidates requires a team of specialists who can pool their knowledge to identify which nerves could potentially be reconstructed or replaced, and which donor nerves might offer the best chance for good outcomes.
Team-based rehabilitation
Patients in our TM rehabilitation program get the full support of a team of specialists who work closely with our neurologists:
- From the very early stages of TM, physical medicine and rehabilitation (PM&R) doctors and therapists help patients learn new ways to move, walk, and care for themselves.
- Our expert urology colleagues, such as Gary Lemack, M.D., provide strategies to manage bowel and bladder symptoms. Dr. Lemack has published on unique aspects of management in patients with neurogenic bladder.
- Psychologists and psychiatrists work with our patients to manage the emotional and social tolls of TM, such as isolation, anxiety, and depression. In partnership with Siegel Rare Neuroimmune Association, we connect patients with support groups and TM educational resources.
- Social workers and school liaisons join the team to help pediatric patients and families navigate new routines at home and school.
UT Southwestern researchers play a major role in informing our care plans with the latest TM advancements. Our patients have access to the most advanced therapy and rehab options, including access to participate in clinical trials that lead to new and refined treatments.
The future of TM care
In collaboration with Nancy Monson, Ph.D., an Associate Professor of Neurology and Immunology at UT Southwestern, the TM team has been investigating the immune profiles of patients with myelitis who were diagnosed with MS in comparison to other conditions. We hope to gain a more thorough understanding of differences in specific proteins in patients’ cells that could be targeted for new or refined treatments.
The TM team is also partnering on a clinical study for a novel treatment approach that combines neurosurgery with next-generation myelin regeneration technology.
Every year, the number of idiopathic myelitis cases declines because we are utilizing new tests developed to determine specific causes of TM, which allows us to create more precise care plans to reduce damage to our internal “wiring.”
As leaders in the research of transverse myelitis, we are committed to advancing the understanding and treatment of this complex condition.
To visit with a transverse myelitis expert, call 214-645-8300 or request an appointment online.











