UT Southwestern’s latest Specialized Program of Research Excellence aims to create new precision interventions to reduce liver cancer incidence and mortality.
More than three decades ago, the National Cancer Institute (NCI) established the first Specialized Program of Research Excellence (SPORE), an initiative that promotes collaborative, interdisciplinary research to move promising cancer discoveries from the laboratory to the clinic. Supported by grants worth millions, institutions chosen as SPOREs use this money to fund translational research projects aimed at fighting these cancers, cores that support that research, and early investigators whose work has shown extraordinary potential.
For years, UT Southwestern’s Harold C. Simmons Comprehensive Cancer Center has been home to two SPOREs, focused on lung and kidney cancers. In September 2025, UT Southwestern was awarded a third SPORE for liver cancer.
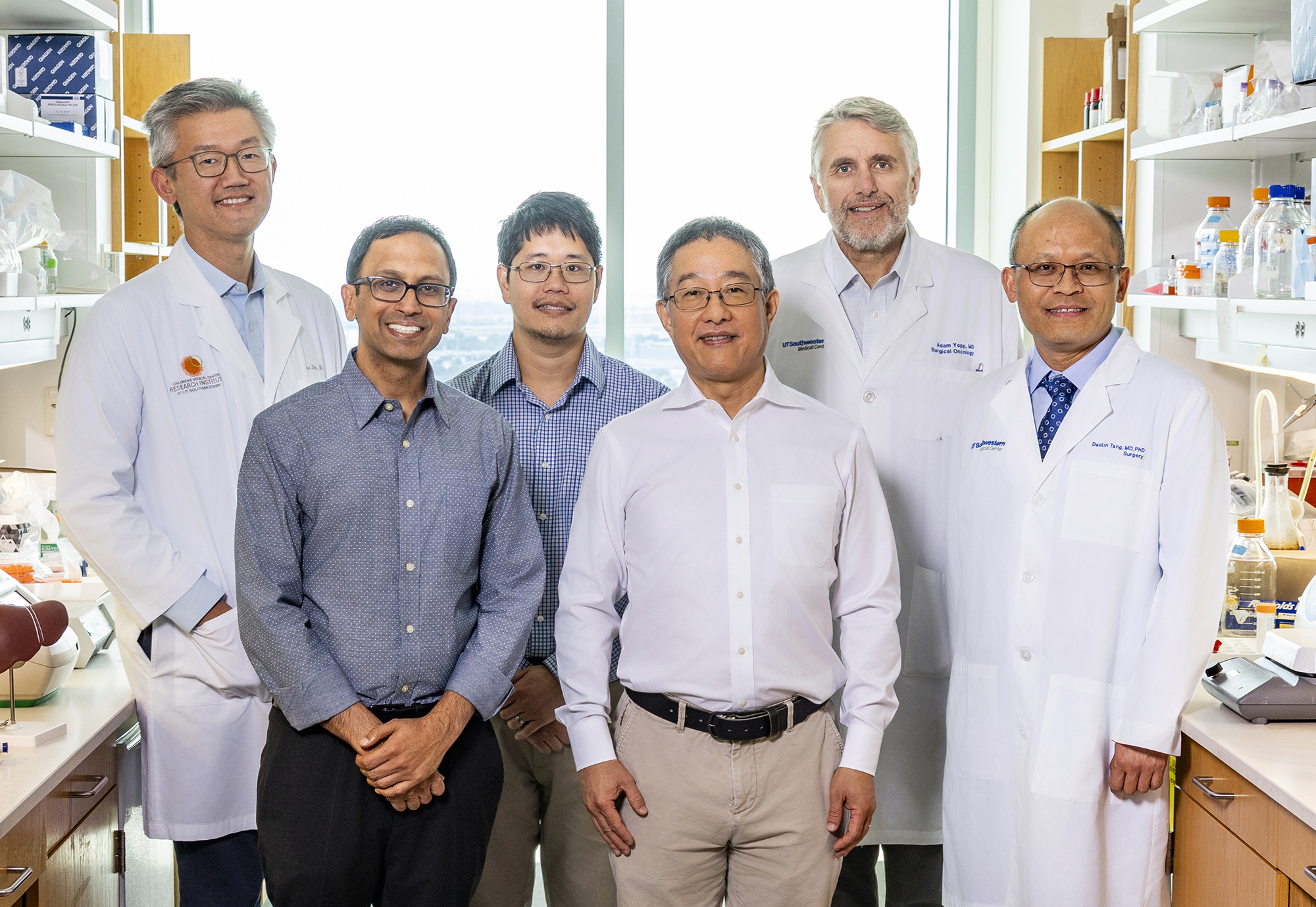
“We’re quite honored to be chosen as a liver cancer SPORE, particularly because we are one of only three sites in the country,” says Amit Singal, M.D., M.S., Professor of Internal Medicine in the Peter O’Donnell Jr. School of Public Health as well as Medical Director of the Liver Tumor Program and Chief of Hepatology at UT Southwestern. “Our selection speaks to the quality of science and the potential for discovery and advances in clinical care at UT Southwestern.” Dr. Singal co-leads the SPORE with Yujin Hoshida, M.D., Ph.D., Professor of Internal Medicine and Director of Liver Tumor Translational Research.
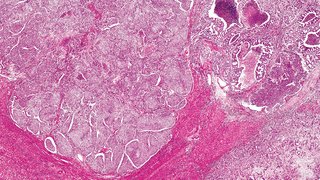
The new SPORE’s overarching goal is to transform innovative scientific discoveries from researchers at the Simmons Cancer Center into precision interventions that reduce liver cancer incidence and mortality. The effort will have a special focus on hepatocellular carcinoma (HCC), which accounts for more than 85% of liver cancer cases across the nation. More than 42,000 new cases of liver cancer, including HCC, are diagnosed every year in the United States, and more than 30,000 Americans die of liver cancer annually. Cirrhosis from heavy alcohol use, metabolic dysfunction, viral hepatitis, and genetic predisposition are key risk factors for HCC and other liver cancers.
These risk factors are particularly common in Texas, which has one of the highest incidences of HCC in the country, Dr. Hoshida says. UT Southwestern joins the Mayo Clinic and MD Anderson Cancer Center as the NCI’s third liver cancer SPORE in the country.
“Our goal is to significantly improve liver cancer survival rates by refining the prevention and treatment of this disease through various new approaches,” he says.
Funded Research
The bulk of the SPORE grant will fund three research projects.
The first, led by Drs. Singal and Hoshida, will test a promising “chemoprevention” strategy in people considered at high risk of developing HCC due to existing cirrhosis. Previous research in animal models at UT Southwestern showed that a protein known as the epidermal growth factor receptor (EGFR) appears to promote cirrhosis-driven HCC growth.
By restricting production of this protein through an EGFR-inhibiting drug called erlotinib, researchers reduced the risk of HCC in these mouse models, a result mirrored in a recent phase I clinical trial in patients with cirrhosis. The UT Southwestern team plans to test this strategy in a larger number of patients in a phase II clinical trial, using a novel biomarker they discovered called a prognostic liver secretome signature as a proxy for HCC risk.
The second project, led by Hao Zhu, M.D., Professor in Children’s Medical Center Research Institute at UT Southwestern and of Internal Medicine and Pediatrics, and David Hsieh, M.D., Associate Professor of Internal Medicine, will focus on preventing recurrence of HCC in cirrhosis patients who were previously treated.
Tumors regrow within two years in about 50%–70% of these patients because the risk factors that caused the initial disease are still present, Dr. Zhu explains. Having extra chromosomes in liver cells — a condition called polyploidy — has been shown to be protective against developing HCC. Previous research in Dr. Zhu’s lab showed that reducing a protein known as anillin can induce polyploidy and reduce development of HCC. The researchers plan to test this strategy in a phase I clinical trial in patients at risk of HCC.
The third project, led by Daolin Tang, M.D., Ph.D., Professor of Surgery, and Adam Yopp, M.D., Professor of Surgery and Division Chief of Surgical Oncology and Surgical Director of the Liver Tumor Program, will focus on improving the efficacy of immunotherapy to prevent HCC recurrence. Although immunotherapy drugs have shown promise in treating advanced stage HCC, their benefit in preventing recurrence after HCC tumors are surgically removed has been unclear.
To boost their performance, the researchers plan to test these drugs in combination with a drug known as a telomerase reverse transcriptase (TERT) enzyme inhibitor. This agent has been shown to selectively stop HCC cells from multiplying and kill them while also activating a cancer-fighting subset of immune cells. A planned phase Ib trial will test the safety and efficacy of the TERT inhibitor combined with immune checkpoint inhibitors in patients who will undergo surgery to remove HCC tumors.
Additional Funding
Along with these projects, the SPORE grant will fund a Developmental Research Program, which will provide seed funding to launch new high-risk, high-reward projects, and a Career Enhancement Program, which will aid early-career scientists and clinicians focused on translational liver cancer research.
Additionally, the grant will support three cores: an Administrative and Outreach Core, which will provide essential administrative services for the SPORE; a Biospecimen and Pathology Core, which will house blood and tissue specimens needed for research; and a Data Science Core, which will provide biostatistical and bioinformatical support to researchers.
“The successful funding of the liver cancer SPORE is a major accomplishment of the Simmons Cancer Center,” says Carlos L. Arteaga, M.D., Director of the Simmons Cancer Center and Associate Dean of Oncology Programs at UT Southwestern. “It represents an outstanding example of the multidisciplinary and collaborative science destined to have a major impact on the prevention and treatment of this lethal disease in the state of Texas and beyond as well as a testament of UT Southwestern’s commitment for translational research.”

About the Experts
Amit Singal, M.D., M.S.
Professor, Internal Medicine and Peter O’Donnell Jr. School of Public Health
Chief, Division of Hepatology
Medical Director, Liver Tumor Program Dedman Family Scholar in Clinical Care
Willis C. Maddrey, M.D. Distinguished Chair in Liver Disease
Member, Population Science and Cancer Control Research Program, Harold C. Simmons Comprehensive Cancer Center
Yujin Hoshida, M.D., Ph.D.
Professor, Internal Medicine
Director, Liver Tumor Translational Research
H. Ray and Paula Calvert Chair in Gastroenterology Oncology in Honor of Udit Verma, M.D.
Member, Experimental Therapeutics, Harold C. Simmons Comprehensive Cancer Center