Demystifying Tumor Biology of Hepatocellular Carcinoma
July 13, 2020
Clinical Trials at UT Southwestern
As an academic medical center, UT Southwestern offers clinical trials that give eligible patients access to the newest therapies. Learn more about clinical trials at UT Southwestern.
Researchers are working to better characterize this malignancy.
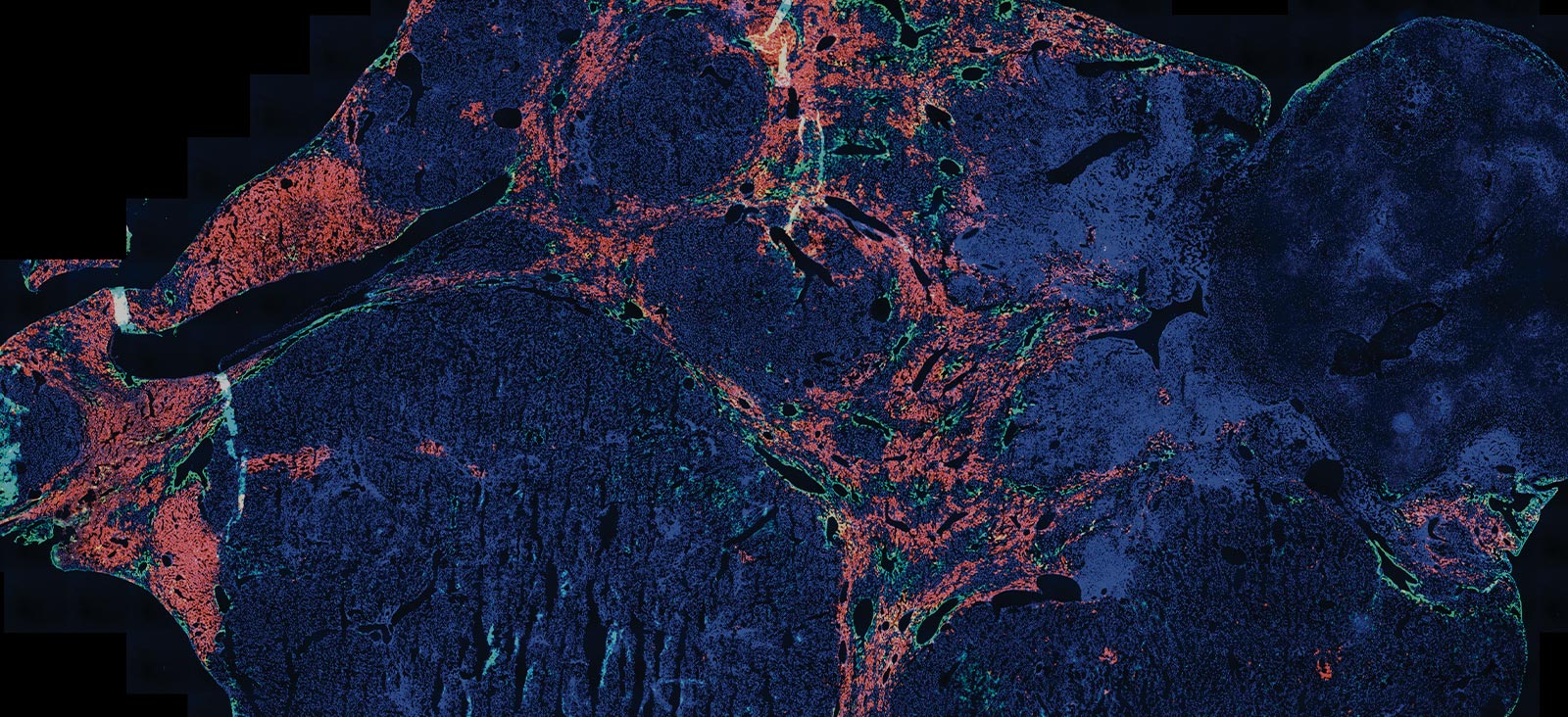
Hepatocellular carcinoma (HCC) is the most common primary hepatic malignancy and one of the leading causes of cancer-related mortality worldwide. [1,2] Despite being one of the most rapidly rising causes of death in the United States, there is a paucity of evidence describing tumor growth patterns, especially in Western nations. [3] Better characterizing HCC growth patterns has several clinical implications, including optimizing screening strategies, prognosis, and treatment decision-making. [2,3]
We’ve noted substantial heterogeneity in prognosis and treatment response for our patients with HCC. However, most studies examining tumor growth patterns were outdated and conducted in patients from other countries, so applying these data to our patients was unclear. As a result, we sought to better characterize the tumor biology and natural history of this cancer in a U.S. population.
Diagnostic Workup and Etiology
The majority of previous data characterizing HCC tumor biology originated from hepatitis B (HBV)-infected patients in Asia. In contrast, the main etiology of disease in Western patient populations is mainly attributable to chronic hepatitis C (HCV) infection and nonviral liver disease, such as nonalcoholic fatty liver disease (NAFLD). [3]
Screening programs for HCC significantly improve early-stage detection of disease and prolong survival, a fact that is continually demonstrated to me as Co-Leader of Simmons Cancer Center’s Population Science and Cancer Control Program and Medical Director of the Liver Cancer Program. However, variation with respect to tumor growth is high, ranging from indolent to aggressive, with the latter form showing significantly worse prognosis. A key component of the workup in patients with positive screening tests involves performing appropriate diagnostic imaging because a diagnosis of HCC can be based on imaging findings in a large proportion of cases. Additionally, the detection of applicable clinical and radiological parameters helps characterize tumor growth. [3]
“Our team at UT Southwestern is leading the field of biomarker discovery and validation for HCC. In addition, we are pioneering several precision medicine strategies to deliver tailored treatment for patients with HCC and other cancers.”
Amit Singal, M.D., M.S.
Recent Findings
As part of several innovative research initiatives at UT Southwestern, we recently conducted a multicenter cohort study to examine tumor growth patterns and characterize tumor biology in a group of HCC patients from the U.S. and Europe. Specifically, we aimed to measure tumor doubling time (TDT) and specific growth rate (SGR), as well as identify factors related to indolent and aggressive growth. [3]
Our primary cohort (n=242) was large and racially and ethnically diverse; the majority of patients were male (87.1%) and had HCV infection (68.3%). We also included a verification cohort (n=176), with similar patient characteristics to our primary group. In terms of tumor growth evaluation, our study is the largest to date among a group of patients with mixed cirrhosis etiologies in a modern Western context. [3]
In our primary cohort, we found marked heterogeneity in TDT (median, 229 days; range, 89–627 days) and SGR (median, 0.3%; range, 0.1%–0.8%). The highest proportion of HCC had indolent growth (38%), 25.2% had aggressive growth, and 36.8% of tumors were classified as having intermediate growth patterns. [3]
Indolent tumor growth was seen more frequently in patients with nonviral cirrhosis compared with viral cirrhosis, larger tumor diameter, and serum alpha-fetoprotein levels of less than 20 ng/mL. [3]
Most surprising was the higher-than-expected proportion of patients with HCC classified as having indolent tumor growth. Our findings highlight the need for novel biomarkers and risk prediction models that can help identify those at highest risk of indolent or aggressive tumors and help tailor treatment decision-making.
On the Horizon
Our team at UT Southwestern is leading the field of biomarker discovery and validation for HCC. In addition, we are pioneering several precision medicine strategies to deliver tailored treatment for patients with HCC and other cancers. We recently helped establish the multicenter Texas HCC Consortium cohort study, with the goal of lowering the burden and mortality of this disease in Texas. Leveraging this prospective cohort, we are evaluating several biomarkers for early detection in patients with liver disease. [4]
Jorge Marrero, M.D., Professor of Internal Medicine and Medical Director of the Liver Transplant Program at UT Southwestern Medical Center, is also leading the National Cancer Institute’s Early Detection Research Network Hepatocellular Carcinoma Early Detection Strategy (HEDS) study, which is actively working on validation of several promising biomarker panels. [5]
Taken together, these cohorts represent approximately 5,000 patients with cirrhosis. We anticipate pivotal results from these studies to be available in the next couple of years, which has the potential to change the way we screen for and manage HCC in the U.S.
About the Author
Amit Singal, M.D., M.S., Associate Professor of Medicine and Medical Director of the Liver Tumor Program at UT Southwestern Medical Center, is an international expert in the detection and treatment of patients with HCC. Currently, Dr. Singal and his team are investigating the underlying mechanisms driving the wide variation observed in HCC tumor biology. [3]
Footnotes
1. Grandhi MS, Kim AK, Ronnekleiv-Kelly SM, Kamel IR, Ghasebeh MA, Pawlik TM. Hepatocellular carcinoma: From diagnosis to treatment. Surg Oncol. 2016;25(2):74-85.
2. Singal AG, Marrero JA, Yopp A. Screening process failures for hepatocellular carcinoma. J Natl Compr Canc Netw. 2014;12(3):375-382.
3. Rich NE, John BV, Parikh ND, et al. Hepatocellular carcinoma demonstrates heterogeneous growth patterns in a multicenter cohort of patients with cirrhosis. Hepatology. 2020 Feb 4. [Epub ahead of print]
4. Feng Z, Marrero JA, Khaderi S, et al. Design of the Texas Hepatocellular Carcinoma Consortium Cohort Study. Am J Gastroenterol. 2019;114(3):530-532.
5. Verma M, Wright GL Jr, Hanash SM, Gopal-Srivastava R, Srivastava S. Proteomic approaches within the NCI early detection research network for the discovery and identification of cancer biomarkers. Ann NY Acad Sci. 2001;945:103-115.