Pancreatic Cancer: Catching It Before It's Too Late
November 8, 2023
Highly experienced, multidisciplinary care team offers hope for patients.
Developing better approaches to prevent pancreatic cancer is becoming increasingly urgent as incidence of the disease rises, particularly among younger patients.
“Pancreatic cancer is not like other cancers, where early detection is associated with long-term survival. Even tumors found in the early stages may be linked with a poor prognosis,” says John Mansour, M.D., Professor of Surgery in the Division of Surgical Oncology at UT Southwestern. “The aim is to identify the precancerous lesions early and remove them before they transform into cancer.”
Dr. Mansour, along with Nisa Kubiliun, M.D., Associate Professor of Internal Medicine, and a team of providers, care for patients in the Pancreatic Cancer Prevention Program at UT Southwestern Harold C. Simmons Comprehensive Cancer Center. The program offers specialized care for those who have been diagnosed with a pancreatic cyst, have an inherited genetic susceptibility, or have a family history of pancreatic cancer.
Benefits of Multidisciplinary Care
A unique aspect of the program is truly multidisciplinary care, which not only offers patients the greatest level of support but also simplifies the many practical issues that arise when battling this disease.
In recent years, studies have shown that pancreatic cancer is frequently associated with inherited gene mutations (e.g., BRCA, ATM, CDKN2A), and the risk of familial disease rises exponentially with the number of first-degree relatives with pancreatic cancer. Current national guidelines recommend genetic counseling and multigene germline testing for all patients with pancreatic cancer.
“Getting a biopsy, going for appropriate scans, consulting with medical genetics, and arranging appointments with multiple experts can take a significant amount of time,” Dr. Kubiliun explains. “At Simmons, we streamline these efforts with care coordinators and patient navigators, which contributes to an efficient and patient-centered experience.”
As a result of the multidisciplinary approach, patients and their families often report feeling much more comfortable, since records and images are collected ahead of time, and all relevant practitioners work together in one place, Dr. Mansour notes.
Delivering a Distinct Care Experience
The pancreatic cancer prevention team then can create a comprehensive surveillance or treatment plan for each patient in a single visit. “With our unique surveillance approach, patients can often avoid chemotherapy and radiation entirely. If we catch it early, we can prevent the disease,” Dr. Mansour adds.
If indicated, patients in the program may be referred to Simmons Cancer Center’s Cancer Genetics Program for a comprehensive evaluation and risk assessment. Genetic testing for pancreatic cancer helps to characterize risk, and genetic counseling gives families information so they understand their options. In most cases, this visit can be coordinated at the same time as their prevention appointment.
“It is often important for first-degree family members to receive genetic testing,” Dr. Mansour explains. “With the results, we can develop a personalized plan tailored to the specific genetic mutation and patient risk factors in accordance with current guidelines.”
Driving Practice Change
There is a paucity of data on optimal practice standards, particularly for individuals at high risk of developing pancreatic cancer, Dr. Mansour says. While current national guidelines recommend that diagnostic management and assessment of resectability of the cancer should involve multidisciplinary consultation at high-volume centers, the most appropriate intervals for imaging studies and the impact of comorbidities (e.g., diabetes) remain uncharacterized.
The team at UT Southwestern is collecting and analyzing data from the program, which started more than five years ago, with the aim of developing protocols that could inform practice globally in the coming years.
Looking ahead, the program’s leaders expect it to remain one of the highest-volume programs in the country that continues to pioneer unique care approaches. “Changing clinical practice is a difficult process, but we’re excited to use our local data to take on that challenge,” Dr. Kubiliun says.
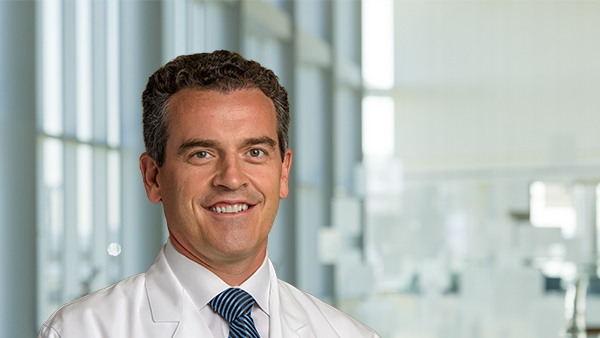
John Mansour, M.D., is a Professor of Surgery, Division of Surgical Oncology, and Vice Chair of Quality in the Department of Surgery at UT Southwestern. He treats patients with malignancies of the stomach, pancreas, liver, bile duct, and other abdominal organs as well as the diverse population of sarcoma patients. Dr. Mansour is a member of the Development and Cancer Research Program at Simmons Cancer Center.
Nisa Kubiliun, M.D., is an Associate Professor of Internal Medicine at UT Southwestern and serves as Clinical Chief of the Division of Digestive and Liver Diseases. She also is the Medical Director of Endoscopy Services, where she employs advanced endoscopic techniques to treat a variety of gastrointestinal disorders and cancers. Dr. Kubiliun is a member of the Population Science and Cancer Control Research Program at Simmons Cancer Center.

Make a Referral
To refer a patient to UT Southwestern Medical Center, call 214-645-4673. Visit here for more information.