Exceptional Care for Acute Pulmonary Embolism
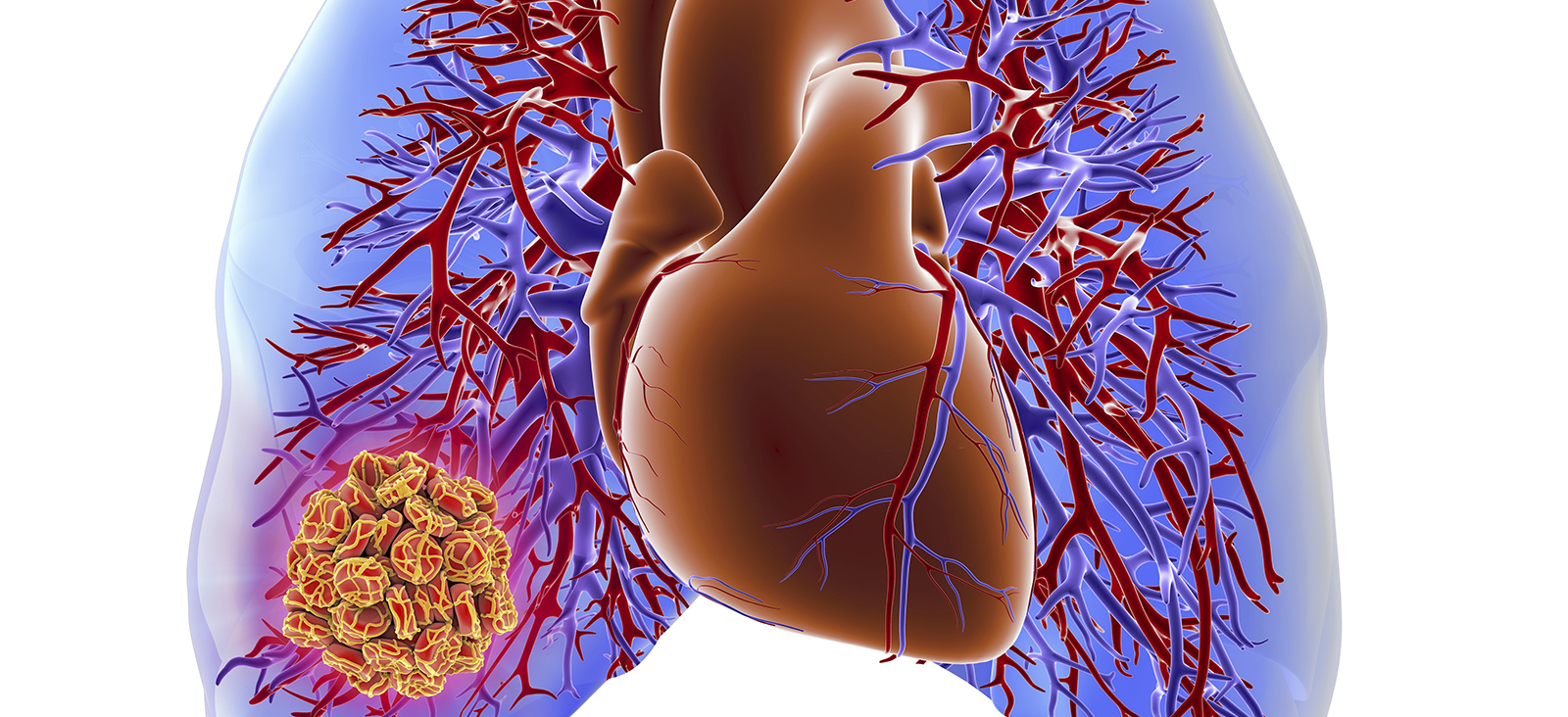
An acute pulmonary embolism, or embolus, is a blockage of a pulmonary (lung) artery. Most often, the condition results from a blood clot that forms in the legs or another part of the body (deep vein thrombosis, or DVT) and travels to the lungs.
Our experienced team of vascular specialists, interventional radiologists, pulmonologists, and cardiologists has extensive clinical and research resources and works quickly to assess and diagnose critical conditions such as acute pulmonary embolism, providing safe, effective treatments that save lives.
Causes and Risk Factors of Acute Pulmonary Embolism
DVT blood clots usually develop in a deep vein of the thigh or pelvis. Most cases of acute pulmonary embolism involve multiple clots that travel from these areas to the lungs but not necessarily all at once. When a lung artery becomes blocked, the areas of the lung the artery feeds don’t receive enough blood and can die. This condition, known as pulmonary infarction, makes it more difficult for the lungs to provide oxygen to the rest of the body.
Blockages in blood vessels can sometimes result from substances other than blood clots, such as:
- Fat from the marrow of a broken long bone
- Collagen or other tissue
- Part of a tumor
- Air bubbles
Anyone can develop blood clots that lead to acute pulmonary embolism, but certain factors can increase the risk, such as:
- Family medical history of blood clots or pulmonary embolism
- Heart disease, especially heart failure
- Inherited disorders that make the blood more likely to clot
- Certain cancers, especially pancreatic, ovarian, and lung cancer, or cancers that have spread (metastatic cancer)
- Surgery, especially bone, brain, or joint surgery
- Long-term immobility such as bed rest or inactivity during long plane or car trips
- Smoking
- Excess weight or obesity
- Pregnancy
- Birth control pills or estrogen therapy
Symptoms of Acute Pulmonary Embolism
Symptoms of an acute pulmonary embolism vary depending on the size of the blood clots, the amount of the lung tissue affected, and whether the patient also has heart or lung disease. The most common symptom is chest pain that:
- Occurs under the breastbone or on one side
- Is sharp or stabbing
- Burns, aches, or feels dull and heavy
- Worsens with deep breathing
Other signs and symptoms include:
- Sudden cough that can produce blood or bloody mucus
- Shortness of breath that starts suddenly during sleep or on exertion
- Dizziness, lightheadedness, or fainting
- Low oxygen level in blood (hypoxemia)
- Fast breathing or wheezing
- Fast heart rate
- Feeling of anxiety
- Leg pain, redness, or swelling
- Low blood pressure
- Low-grade fever
- Clammy or bluish skin (cyanosis)
An acute pulmonary embolism can be life-threatening, so people who experience these symptoms should seek immediate medical attention. The condition can also lead to pulmonary hypertension, which is high blood pressure in the lungs and right side of the heart. In rare cases, the clots do not dissolve over time and become “scarred” in the blood vessels of the lung, causing chronic thromboembolic pulmonary hypertension.
Diagnosing Acute Pulmonary Embolism
Our cardiovascular specialists conduct a thorough evaluation, which begins with a:
- Physical exam
- Review of personal and family medical history
- Discussion of symptoms
We have extensive experience in evaluating and diagnosing acute pulmonary embolism, which can be difficult to diagnose in people with heart or lung disease. To confirm a diagnosis, we usually order one or more tests, such as:
- Blood tests: We measure levels of oxygen, carbon dioxide, and a clot-dissolving substance called D-dimer, as well as check for an inherited clotting disorder.
- Duplex ultrasound: Our technician scans the legs to check for blood clots in the veins.
- Spectral CT angiogram: We use a scanner that takes clear images of the lung tissue and blood vessels to determine where the clots are and how they are affecting lung blood flow.
- Magnetic resonance imaging (MRI): This type of imaging uses a magnetic field and radio waves to produce images, avoiding the use of radiation in X-rays and CT scans.
- Chest X-ray: Blood clots cannot be seen with X-rays, but these images can rule out other conditions with similar symptoms.
Treatment for Acute Pulmonary Embolism
The goal for treatment is to stop the clot’s growth and prevent more clots from forming. Our experienced heart and lung specialists work quickly to prevent serious complications, using the latest treatment options, such as:
- Anticoagulants: We prescribe blood-thinning medications such as warfarin, heparin, or novel oral anticoagulants (NOACs) to prevent new clots.
- Thrombolytics: In life-threatening cases, we can inject clot-dissolving medications to quickly dissolve clots.
- Clot removal: Our doctors can remove clots in emergency situations using a catheterization procedure. When the catheter reaches the blood clot in the lung artery, we can either use an instrument to break up the clot or deliver clot-dissolving medication.
- Vena cava filter: For people who cannot take blood thinners, we can use a catheter to place a filter in the body’s main vein (the inferior vena cava, which leads from the legs to the heart), preventing clots from traveling to the lungs.
Support Services
UT Southwestern’s cardiac rehabilitation specialists create customized plans that integrate proper nutrition, exercise, and, if necessary, nicotine cessation into patients’ lifestyles to improve their vascular health.
Clinical Trials
As one of the nation’s top academic medical centers, UT Southwestern offers a number of clinical trials aimed at improving the outcomes of patients with heart and vascular disease.
Clinical trials often give patients access to leading-edge treatments that are not yet widely available. Eligible patients who choose to participate in one of UT Southwestern’s clinical trials might receive treatments years before they are available to the public.