Why Choose UT Southwestern for a Lung Transplant?
UT Southwestern’s skilled Lung Transplant team uses the most sophisticated tools and techniques to help patients with end-stage lung disease who have exhausted their other treatment options. Our experienced team of experts collaborates to deliver world-class, evidence-based care.
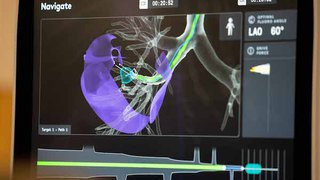
We also pioneer the use of leading-edge technologies to treat patients with advanced lung disease.
UT Southwestern is one of fewer than two dozen U.S. centers using ex vivo perfusion, which helps physicians more thoroughly evaluate donor lungs and aims to improve their quality – expanding the number of available healthy lungs – before they are considered for transplantation. The technology runs artificial blood through the circulatory system of a lung after it has been removed from a donor’s body, thereby extending the time that the lung is viable for evaluation and transplantation.
We also offer extracorporeal membrane oxygenation (ECMO), an established technology that is used outside the body to help diseased lungs and hearts more effectively deliver oxygen to the blood. ECMO allows patients to be mobile, which helps them remain as strong as possible while they await lung transplantation.
Clinical trials help patients access the most promising new treatments before they are available to the public. Patients with lung disease should speak with their doctor to find out if taking part in a clinical trial might be right for them.
Multidisciplinary, Comprehensive Lung Care
Our team includes pulmonologists (lung doctors), surgeons, intensive care physicians, and specialized nursing staff, as well as imaging and infectious diseases specialists, transplant coordinators, social workers, nutritionists, pharmacists, and financial coordinators.
These specialists work together to provide ongoing medical management and simplify every step of the process – from support for patients awaiting lung transplants to comprehensive outpatient treatment of transplant recipients.
For our patients’ convenience, UT Southwestern has regional clinics in Lubbock and Tyler that allow us to perform an initial screening – close to patients’ homes – to see if transplant is an option for them.