One year after the first case of COVID-19 was confirmed in the Dallas-Fort Worth area, we’re entering a new and hopeful phase in the pandemic. Vaccination rates are on the rise, confirmed case numbers are declining, and the Centers for Disease Control and Prevention (CDC) recently issued guidance on what activities are safe for people who have been vaccinated.
But there continues to be some confusion and mixed messages surrounding the virus and its ongoing potential to spread. Recently, I had the opportunity to discuss the state of the pandemic, the vaccines, the virus variants, and the need for ongoing public health measures with Dr. John Warner, UT Southwestern’s Executive Vice President for Health System Affairs, for an episode of his online web series “What to Know.” We tried to answer many of the frequently asked questions we’re hearing at UTSW about the vaccines and reiterate one important fact:
COVID-19 is not gone yet, regardless of how much we’d all like it to be. Unfortunately, we can’t just flip a light switch and return to normal. Think of the pandemic as being on a dimmer, and we're starting to bring up the lights, particularly for individuals who are fully vaccinated. But we’re not yet to the point where we can fully turn on the lights in the room.
Below is an edited version of our “What to Know” conversation, primarily focused on what you can and can’t do following vaccination.
Life After Vaccination
More people are getting vaccinated against COVID-19 and wondering what’s next in this new phase of the pandemic. Dr. Brad Cutrell, an infectious disease specialist at UT Southwestern, answers some of the big questions about what’s safe post-vaccination.
What are some safe activities for vaccinated patients, according to the CDC?
First, we should define “fully vaccinated:” That means two weeks after you've received the second dose of one of the mRNA vaccines, Pfizer or Moderna, or two weeks after receiving the one-shot Johnson & Johnson vaccine.
For those individuals, the CDC guidelines state it is safe to gather in a private or home setting with another group of individuals who are fully vaccinated without wearing masks or practicing physical distancing. You can also be around people who are unvaccinated, who are not at high risk of severe illness from COVID-19. The third important thing is that you no longer have to quarantine or get tested if you're asymptomatic following an exposure.
What’s the definition of someone who's at low risk?
That includes people under the age of 65 who don't have an underlying medical condition that puts them at risk of being hospitalized from a COVID-19 infection. Heart disease, obesity, and diabetes are among those conditions, so anyone who has one of those conditions, who's not yet vaccinated, we need to be more cautious around them.
What's your advice for people who work in small settings with vaccinated individuals?
When you are exclusively around people who are fully vaccinated, then you can probably set the masking aside. However, if you're in a situation where there may be a mixture of people who are vaccinated and unvaccinated from multiple households, that's where you really need to still practice masking and physical distancing.
In what other situations should fully vaccinated people still wear a mask and physical distance?
When you're out in public, in medium to large group gatherings, or in situations where there is a mixture of people who are vaccinated and unvaccinated, that's really where you should continue to wear a mask and watch your physical distance until a larger percentage of the population gets their vaccine.
This is spring break season. Is it safe to travel?
The CDC hasn't changed its travel recommendations, so you should probably consider carefully whether to go on non-essential travel. If you do travel, consider driving rather than taking public transportation. Once you get to your destination, think about who you are going to be around. Private gatherings with vaccinated family members are going to be safer.
If you travel internationally, remember that you are required to get a COVID test before you come back and a seven-day quarantine is recommended, even if you're fully vaccinated.
What’s the difference between the Pfizer, Moderna, and J&J vaccines?
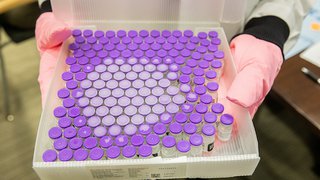
All three vaccines target the spike protein of the SARS-CoV2 virus, which enables it to attach to and invade cells in our bodies. The vaccines don’t contain a live virus, so you can’t get COVID-19 from any of them. Also, the vaccines have all proven very effective at preventing severe cases of COVID-19 that would lead to hospitalization and death. They all met and exceeded the FDA's requirements for safety and effectiveness.
All three are very good vaccines, but there are some differences. The mRNA vaccines, Pfizer and Moderna, are two-shot vaccines. They have stricter cold storage requirements. And in clinical studies, they were 94 to 95 percent effective at preventing milder disease. These results were from clinical trials that were conducted in the fall.
The J&J vaccine is what we call an adenovirus vector vaccine, which means it contains a harmless, engineered virus that can't cause disease, and it gets shuttled into the cell to prompt the immune response. J&J is a one-shot vaccine that can be stored at refrigerator temperature for much longer, so it’s easier to distribute. Clinical trials were done in the winter, at the peak of the pandemic, and they still showed the vaccine to be about 67 percent effective against milder infection.
It’s difficult and probably unwise to compare the vaccine trials against one another. The conditions and community spread were very different. We're recommending that people get whichever vaccine is offered to them first because all three are very effective at preventing serious COVID-19 illness.
Are there certain people who should get one vaccine versus the other?
If someone has had an allergic reaction to one of the COVID vaccines, then for their next dose, they should talk to their physician about getting one from the other vaccine classes. There also may be certain situations where an individual isn’t going to be able to return for a second dose, so they may prefer at the start to get the J&J single-dose vaccine. Other than that, the vaccines are broadly similar and effective across a diverse population – including age, race, ethnicity, and different medical conditions.
Are there differences in how long the vaccines’ protection lasts?
We have very good evidence for all the vaccines that they provide robust protection for at least three months, because that's how long the trials followed individuals. Beyond that, we do think the vaccines will offer longer protection. We just don't know how long. Will it be six months? A year? The vaccine companies are already looking at the possibility of adding a booster vaccine to help increase the longevity of that immune protection, or to help target some of the viral variants that are out there.
Explaining mRNA vaccines
The Pfizer and Moderna vaccines use mRNA technology to help create immunity from the SARS-CoV2 virus that causes COVID-19. What is an mRNA vaccine and how does it work? UT Southwestern explains.
What is a variant and why is there concern about those?
A variant is a virus strain that has accumulated enough mutations that there is some difference either in how contagious or infectious it is, or in the type of disease it causes. There are a number of circulating variants, such as the one first identified in the U.K. The vaccines appear to be very effective at preventing disease with that variant. With the so-called South African variant, there is diminished effectiveness but the vaccines still provide enough protection to prevent serious disease. This is an area that many of us in the scientific community are actively tracking, including here are at UT Southwestern.
When do you think we'll have enough vaccine for everyone regardless of their risk or medical conditions?
This is an area where I think we have some really hopeful news. With the emergency use authorization for the J&J vaccine, as well as several steps that have ramped up production of the Pfizer and Moderna vaccines, the latest estimates are that by the end of May we’ll have enough vaccine for any adult in the U.S. that wants to get the vaccine. So that's very encouraging news.
I think for older adolescents, it may be fall before we have the data as well as the supply of vaccine to get them vaccinated. And for younger children, it could be the beginning of 2022 before the vaccines are authorized for them because we really need to wait for the safety and effectiveness data.
What would you say to people who have been waiting to get the vaccine?
I think the most encouraging thing is that we have great data from the clinical trials, and when we rolled the vaccines out in the real world they stood up to the test and have been equally effective. A number of studies from hospitals and health-care settings, as well as early-adopter countries such as Israel, have shown these vaccines are very effective at preventing disease, really at the level we saw in the clinical trials, which is very encouraging. That has been our experience at UT Southwestern as well.
There's increasing data showing the vaccines are also about 75 to 80 percent effective or more at preventing asymptomatic infection as well, which is something we didn't know for sure a few months ago from the clinical trials.
What advice would you give to people who have been vaccinated about going to shopping malls and larger venues?
For those who are fully vaccinated, it’s OK to consider selectively going to some of those areas, but when you do that, that would fall into the public setting. So you should still practice all of the precautions of wearing a well-fitting mask, practicing physical distancing, and avoiding large gatherings.
What do you say to people who are still hesitant to get the vaccine?

The first thing I say is I understand. These are new vaccines and people have lots of questions, but I've looked at all of the science and I've taken the vaccine myself. Vaccines are the most effective tools we have to get out of this pandemic – they are the path back to gathering with our loved ones and doing things we love to do.
I strongly encourage everyone to get answers to their questions from medical professionals, but ultimately, I think getting the vaccine when you have an opportunity is the right choice.