COVID-19 and flu: Navigating a potential ‘perfect storm’ this fall
September 30, 2020

In a normal year, flu activity usually begins to increase in October and November and peaks between December and February. But 2020 has not been a normal year.
Since spring, this year has been dominated by the coronavirus and its social ramifications. Now that fall has arrived, it’s a fair question to ask whether we should be bracing for a collision between flu season and the COVID-19 pandemic – and, in fact, how worried should we be this year about facing a double pandemic?
We recently appeared on an episode of “What to Know,” UT Southwestern’s weekly web series, where we discussed the upcoming flu season, how COVID-19 would affect it, and how patients, parents, and children can prepare for what some are calling a “perfect storm” of respiratory viruses. Some of the highlights of that discussion follow.
What is the primary concern heading into this flu season?
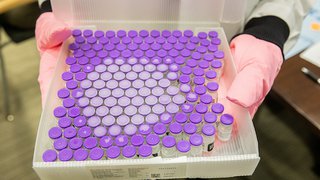
Dr. Trivedi: We are concerned about the potential for increased numbers of cases of influenza this year compared to years past. We’re looking for ways that we can minimize our risks of coming down with influenza and other respiratory viruses, as well as making sure in hospital settings and doctor’s offices that we have ways to test for influenza as well as, potentially, for COVID-19.
Are the pediatric guidelines for flu prevention and vaccination any different this year?
Dr. Sue: The American Academy of Pediatrics (AAP) recommendations emphasize many of the same points that have been raised previously, namely that children 6 months old and older need to be vaccinated. In the setting of the COVID-19 pandemic, there is even more urgency to do so to prevent co-infection and additional morbidity and mortality.
If someone gets the flu, is it more likely they could also get COVID-19 or, vice versa?
Dr. Trivedi: I don’t think we truly know just yet. There have been mixed predictions both ways about what we might expect for the upcoming flu season. Currently in the U.S., we are still reporting anywhere from 30,000 to 40,000 cases of COVID-19 per day, and there is some concern that if we are seeing these high rates that it could mean that people are still engaging in the same types of behaviors that might put them at risk for acquiring influenza, such as being in close proximity to other people or showing up to events or work or school when they are ill. Meanwhile, there are also other predictions on the other side saying that if we do adhere to the nonpharmacologic interventions that we’ve been talking about and that we know are so important for COVID-19 prevention – masking, social distancing, hand hygiene, limiting interactions with other people – we might actually see a better flu season compared to years past. So, it’s a little bit up in the air.
What advice are you giving to parents to keep themselves and their children safe?
Dr. Sue: We know that children, because of their social behaviors are at much higher risk for illness due to influenza than older adults – they have a much higher “attack rate,” as we call it. Children are also key entry points for household spread. If you are able to prevent a child from bringing influenza into the home, the risk of others in the house of being infected drops. So, prevention is the No. 1 priority here, and the first step is vaccination. Flu vaccine makes a huge difference in children, and reduces the risk of hospitalization by up to 50%. So we are encouraging our patients to, first, make sure your child is vaccinated, and, second, to continue distancing and masking, because flu is a respiratory virus that spreads in the same way as COVID-19.
When is the right time to get your flu vaccine?
Dr. Trivedi: Here at UT Southwestern, we began offering it to our patients and employees as of mid-September. Between now and the end of October is probably the ideal time to be vaccinated. It takes about two weeks for your body to be able to build up immunity to the flu vaccine. That being said, though, even if it’s after October 31, it’s still not too late to receive your flu vaccine.
COVID-19 + Flu: Dual Threats
This fall we’re bracing for a flu season like no other due to added concerns about COVID-19. Dr. Julie Trivedi, Medical Director of UT Southwestern’s infection prevention efforts, and Dr. Paul Sue, a pediatric infectious diseases specialist, size up the looming “perfect storm” and offer practical advice to stay safe.
What's the difference between a nasal vaccine and a flu shot, especially for kids?
Dr. Sue: The nasal vaccine is what we call a live-attenuated vaccine, which uses a live but weakened (or “attenuated”) form of the flu virus. Children less than 2 years old, or anyone with (or living with someone who has) an immunocompromising condition, should not receive the nasal vaccine. However, in otherwise healthy children, the American Academy of Pediatrics considers the nasal vaccine and the inactivated vaccine – the shot – to be equally effective this year and recommends either option for most children.
For adults, who should get a regular-dose versus a high-dose vaccine?
Dr. Trivedi: Both of those vaccines are “quadrivalent,” which means they contain antigens against four strains of influenza. The high-dose version contains four times the amount of antigen as the regular vaccine and is recommended for individuals over the age of 65 to help boost their immune response to the vaccine. Studies have shown that the high-dose type is protective against developing flu as well as flu’s more severe complications. Individuals should discuss with their primary care provider about receiving the high-dose vaccine if they’re over age 65.
If someone has COVID-19 or flu and has recovered, how long are they infectious?
Dr. Trivedi: The incubation period for influenza is anywhere from three to four days, and then people usually remain infectious for about five days. So once their fever resolves and they have had an improvement in their cough and have been treated with Tamiflu, we no longer consider them infectious, and they are able to return to the work environment, if in fact they had only influenza. For COVID-19, what we know is that after exposure, symptoms usually present in anywhere from two to five days but can take up to 14 days to develop.
Based on guidance from the CDC, when we look at clearing individuals with infection, there are two things that we consider: One is the severity of illness, and that helps us determine what duration they might be infectious, and then the other thing is the resolution of the fever and symptoms. In general, for most individuals who’ve been infected with COVID-19 who are out in the community and maybe are requiring very minimal amounts of oxygen, they may be infectious for 10 days. Individuals who are more severely ill and in the hospital, such as in the intensive are unit, might be infectious for 20 days or longer.
When is the best time for someone with flu symptoms to take Tamiflu?
Dr. Trivedi: Ideally, Tamiflu or any of the other flu medications, should be started as soon as possible after symptom onset or diagnosis. Studies have shown that initiation of these medications within the first 36 to 48 hours – sometimes up to 72 hours – is really crucial to help minimize shedding of the virus in the environment, as well as to shorten the duration of symptoms.
What would you say to someone who is unsure about getting a flu vaccine this year?
Dr. Trivedi: It’s really important that people address these concerns with their primary care provider so they can receive appropriate and clear guidance and information about what types of things to expect. If one were to then receive the flu vaccine, we know that some common side effects are soreness at the injection site, maybe a low-grade fever, and feeling a little fatigued for a day or so after receiving the vaccine. It’s really important this year, though – even more important in light of COVID-19 because not only does it help to prevent you from becoming infected with influenza but then even if you actually were infected with influenza, we know that the severity of your illness will be milder.
Your symptoms will be a lot milder than if you did not have the vaccine. Past studies have shown when we have looked at individuals who have died of influenza or influenza complications were not vaccinated.
What are three things you recommend for parents this flu season?
Dr. Sue: As our mantra for flu season this year, we are emphasizing the basics. Influenza vaccination, social distancing and masking, especially in the age of COVID-19, and making sure that everyone is washing and keeping their hands clean, especially after touching their faces and noses!
For more information on COVID-19 and the 2020-21 flu season from UT Southwestern’s experts, please visit the MedBlog or utswmed.org/covid-19.