The global COVID-19 pandemic has encroached on nearly every aspect of our lives in the last few months, creating an insatiable appetite for fresh information about the coronavirus.
We all have questions, such as:
- What’s the best way to protect myself and my family?
- Will COVID-19 be a seasonal infection and go away by summer?
- Is there a quick way to build up immunity to the virus?
And we’re all searching for answers.
But amid the torrent of media coverage from legitimate sources and less reputable outlets, facts can often get obscured by fiction or false hopes. Myths begin to rival realities.
The World Health Organization (WHO) has even dubbed the phenomenon an “infodemic.”
With that in mind, we’d like to address some of the misconceptions swirling around COVID-19. These answers may not necessarily be the ones you want to hear, but they are based on evidence and firmly rooted in science.
Myth:
Groceries and restaurant deliveries all need to be wiped down or sanitized.
Reality:
The risk of obtaining COVID-19 from food or grocery packages delivered to your house is very low.

Epidemiologic literature has shown that food packaging is not a major mode of spread. As a respiratory infection, COVID-19 is most commonly spread via respiratory droplets so the bigger risk in obtaining groceries or having food delivered is the contact with other human beings who may be sick. In those cases, stay six feet away from others as much as possible in the store/pickup line, avoid touching your face, and wash your hands for at least 20 seconds before and after coming into contact with people in public.
However, if you are concerned, you can add an extra layer of protection by picking up the delivery packages with gloves, disposing of the outer packaging, then disposing of the gloves and washing hands. Also, putting delivery food (in oven-safe containers) in at least a 170-degree oven for 20 minutes will minimize infectious particles. This method is occasionally used as a protocol for sterilizing health care workers’ masks.
Myth:
COVID-19 can live for several weeks on packages or mail.
Reality:
You are much more likely to catch the virus from the air, standing next to a sick person than from a package, a piece of mail, or a surface.
A study published in the New England Journal of Medicine reported that the virus can live up to 72 hours on plastic, 48 hours on stainless steel, and 24 hours on cardboard. Although that may sound alarming, the amount of virus that remains is very small, with 0.1% of the starting virus material still on the plastic at 72 hours, for instance. Nevertheless, the CDC recommends you clean high-touch surfaces in your home such as doorknobs, sink handles, desks, keyboards, and tables.
Myth:
The summer heat will put an end to the spread of the novel coronavirus.
Reality:
There is no scientific basis to believe summer weather, more intense sun, or increased humidity will have a dramatic effect on the spread of COVID-19.
The National Academies of Sciences, Engineering, and Medicine recently sent a report to the White House and cited several studies that confirmed this conclusion. Ongoing mitigation strategies such as social distancing and shelter-in-place orders will likely be the cause of reduced spread if it occurs in summer months. The report also points to hot climates in Australia and Iran, both of which experienced rapid spread of the viruses during periods of warm weather, as reasons why COVID-19 won’t behave the same way as seasonal outbreaks such as influenza.
A candid conversation about COVID-19 testing
UT Southwestern's Dr. Julie Trivedi, an infectious disease expert, is featured in the debut episode of 'What to Know,' hosted by Dr. John Warner, Executive Vice President for Health System Affairs. They discuss a range of topics, including COVID-19 testing, new mask protocols, and when life may begin to return to normal.
Myth:
Once you catch COVID-19, you are immune from catching it again.
Reality:
No reputable health expert has suggested that would work.
Some erroneous reports have suggested that if a certain number of Americans were to expose themselves to the coronavirus they would develop valuable antibodies necessary to ward off reinfection and become a kind of “immune elite,” able to return to work and rescue the American economy. Typically with a viral illness, if a patient recovers from it they build up immunity, but some viruses are able to change over time and overcome that immunity. That’s why influenza returns every year in a slightly different form. We aren’t sure yet what will happen with this novel coronavirus. In fact, the WHO is investigating reports from South Korea of prior COVID-19 patients getting reinfected – totally contradicting the “herd immunity” theory.
Myth:
Several medications are effective in treating and preventing COVID-19.
Reality:
No pharmaceutical options have been approved by FDA.
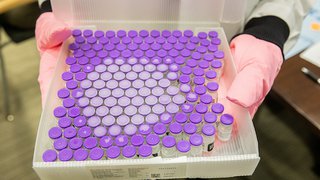
And while efforts to create a vaccine are ongoing, the Centers for Disease Control and Prevention (CDC) estimates it will take 12-18 months before one might be readily available. Clinical trials are investigating several drugs, such as the intravenous antiviral medication remdesivir and hydroxychloroquine, a pill used for treating malaria. But neither has been proven effective (or safe) yet. The best use of those agents is in a clinical trial protocol so we can determine their safety and efficacy. We have those protocols at UT Southwestern. There have been reports of people using fish tank cleaning products that contain chloroquine phosphate to treat COVID-19, but those products are not intended for human use and can be poisonous if not used correctly.
Interleukin-6 is a protein associated with excessive inflammation in the lungs and body in severe infections and has been shown to be activated in COVID-19 patients. Sarilumab and tocilizumab are monoclonal antibodies (or blockers) to Interleukin-6, and the effect of these drugs on COVID-19 is still being studied.
The U.S. Food and Drug Administration has approved investigational use of convalescent plasma, which can be donated by somebody who has recovered from COVID-19 and has built up antibodies to the virus in hopes their plasma will stimulate a stronger immune response in a patient still battling the infection. UT Southwestern is accepting donations of convalescent plasma, and this therapy has shown some early promise, but there isn’t enough data yet to be conclusive.
Myth:
Vitamins or superfoods can quickly boost your immunity to COVID-19.
Reality:
That’s a common misconception.
There is no food, supplement, or “magic bullet” nutrient to automatically boost your immunity to viruses such as the novel coronavirus and any related respiratory infections. Eating garlic, for instance, is considered healthy, but there is absolutely no evidence it will protect you from contracting COVID-19. Strengthening your immune system through a healthy diet, regular exercise, and mental health care is the most effective strategy. Certain foods are good for the immune system, and building a healthy diet begins with focusing on what we eat and our relationship with food.
Myth:
'Superspreaders' can infect large groups of people with COVID-19.
Reality:
There is no evidence of a turbocharged strain of the virus.
R0, or R naught, is a mathematical measurement of how contagious a disease can be, and COVID-19 has an R0 of about 2 to 2.5, which means each new infected person spreads it to about 2.2 people on average. That is higher than the flu, but experts believe the spread can be controlled by social distancing and other mitigation strategies. The only known way one person can infect a large group is by violating those guidelines.
Myth:
Hair dryers, hot baths, and saunas can ward off the new coronavirus.
Reality:
That's a lot of hot air.
A viral video suggesting that using a hair dryer to blow hot air up your nose to prevent or cure COVID-19 represents a basic misunderstanding of how respiratory illnesses advance. The coronavirus does not just sit idle in your nasal passages or throat. Viruses invade normal cells and use those cells to multiply. And hot water doesn’t begin to kill bacteria until it reaches at least 140 degrees – a temperature that would scald your skin. That’s one reason proper handwashing recommendations don’t include using hot water. The CDC has also said there is no evidence COVID-19 can be spread to humans through the use of pools, hot tubs, or spas as long as they’re properly maintained. Disinfectants such as chlorine and bromine should inactivate the virus that causes COVID-19.
Myth:
Drinking alcohol, colloidal silver, or copious amounts of warm water can kill some strains of COVID-19.
Reality:
None of these will prevent or kill COVID-19 infections.
Drinking alcohol can actually be dangerous to someone with the virus. Same goes for colloidal silver, which has been the subject of bogus medical claims. Ingesting liquids with silver can cause kidney damage, seizures, and a condition that makes your skin turn blue. Drinking water is good for your health, but there is no evidence drinking a glass of warm water every 15 minutes or gargling with saltwater regularly has any effect on COVID-19.
Myth:
Young people are not at risk of getting COVID-19.
Reality:
No age group, race, or ethnicity is immune.
People over age 65 and patients with pre-existing medical conditions (most commonly asthma, diabetes, and heart disease) are considered to be at higher risk, according to the data. But there have been many instances of young people getting the virus. And among those ages 20 to 44 with COVID-19 in the U.S., nearly 20% were hospitalized, according to the CDC. The Washington Post recently reported that more than 750 people under age 50 have died from COVID-19 as of April 8, with at least 235 of those victims being in their 20s and 30s.
Help stop the spread of rumors, panic
Our best defense against COVID-19 is to work together and follow the physical distancing and prevention guidelines that have helped flatten the curve so far. The same is true for misinformation. Together we can slow its spread, too.
The Federal Emergency Management Association has created a rumor control website that can help delineate fact from fiction. The WHO has also created a “Myth Busters” website, complete with graphics and video, to rule out some of the more outlandish and conspiratorial claims, such as:
Myth: 5G mobile networks are spreading COVID-19.
Reality: Viruses are incapable of traveling via radio waves or any kind of mobile network.
Myth: If you can hold your breath for 10 seconds without coughing, you are free of COVID-19.
Reality: A valid lab test, which involves a nasal swab or blood sample, is the only way to confirm who has – or doesn’t have – the disease.
Myth: Mosquitoes can help transmit the novel coronavirus.
Reality: Despite the fact that mosquitoes spread West Nile and malaria, there is no data showing the pests transmit the coronavirus, according to the WHO. (COVID-19 is believed to have originated from an animal market in Wuhan, China, and was spread by bats to humans.)
If you want to help prevent the spread of the current “infodemic” of false claims about COVID-19, be diligent about checking the source of the information before you share it. Major health organizations such as the CDC and WHO are among the most credible sources on the COVID-19 pandemic.
So are academic medical centers, such as UT Southwestern. We are providing regular updates on COVID-19 and our response to the virus at utswmed.org/covid19. You can also find answers to more of your questions at utswmed.org/medblog.