Over the course of a year, we have experienced the ups and downs of the COVID-19 pandemic – from fear to frustration, loss to hope.
Even the excitement surrounding the delivery of highly effective COVID-19 vaccines has been tempered somewhat by the emergence of several variants of the SARS-CoV2 virus that were first identified in the U.K., South Africa, and Brazil.
As these variants have spread around the world, some scientists and news outlets have warned we are now in a race to vaccinate enough people before the constantly evolving virus eludes the immune responses created by vaccines. How much of a race we are in remains unclear.
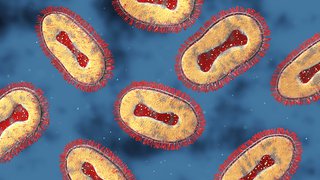
Viruses have been mutating for millions of years, and we knew SARS-CoV2 would likely produce thousands of variants, most of which have little to no impact on the severity of disease in humans. For the few variants that do have the potential to increase transmissibility or skirt some of the antibodies created by vaccines, sequencing becomes a critical public health tool so we can monitor them it in real time and respond quickly if needed.
We are doing some of that important work here at UT Southwestern, and recently I joined Dr. John Warner, Executive Vice President for Health System Affairs, to discuss this topic of variants on his video series “What to Know.” Below is an edited transcript of our discussion, with some updates on the evolution of the variants.
What is a COVID-19 variant and why should we be concerned about them?
Viruses, particularly RNA viruses like SARS-CoV-2, evolve and when they do, they make mistakes or typos in their genetic code. That’s totally normal and expected. We see that with other viruses such as influenza, and that’s one of the reasons we get a yearly vaccine for flu because the virus is constantly changing.
The same is true for the virus that causes COVID-19, and these genetic changes create what we call variants. Sometimes variants are completely inconsequential. And sometimes they impact how the virus is transmitted. The variants we’ve been seeing lately fall into that category and raise questions about what it means to have them circulating in the community.
How many variants are we seeing and what are the differences between them?
Thousands of variants have already been documented. The U.K. variant has been in the news a lot partly because of how rapidly it has been detected there and how quickly it has spread. On April 7, the Centers for Disease Control and Prevention (CDC) announced that the U.K. variant, also known as B.1.1.7, has become the dominant strain of the virus in the U.S. The issue with this particular variant, along with those found in Brazil and South Africa, is that they share some common features, but they're not identical. The worry about all of them is whether this means we're about to enter a phase where this virus could transmit even more easily.
| Variant name | Origin | Effects on spread | Effects on vaccine |
|---|---|---|---|
| B.1.1.7 | First identified in the U.K. 12/20 | ~40% more transmissible | *Vaccines appear to be effective against it |
| B.1.351 | First identified in South Africa 12/20 | Heightened transmissibility | *Unclear if vaccine potency is weakened |
| P.1 | Discovered in travelers from Brazil | No proof it is more transmissible | *No data to suggest it weakens vaccine |
*The effect of certain variants on vaccine performance is likely to be vaccine specific. So far, the mRNA-based vaccines that are being used in the U.S. appear to be holding up well against concerning variants.
Do variants cause more severe disease?
Not necessarily. The variant may be a bit more infectious or transmissible because it is able to bind better to cells or enter them more efficiently. Those are characteristics that give the variants a small advantage over the original virus. Over time, as more people have been infected, these small differences in the population can become bigger differences. But, so far, the variants haven’t produced more severe COVID-19 illness and the vaccines continue to show high efficacy against these new strains.
What is sequencing and why is it important?
Sequencing, which is essentially decoding the DNA or RNA building blocks of a virus, is being done on a larger scale in the U.S., and it is also happening here in North Texas. I oversee the microbial genomics lab within the Infectious Diseases division at UT Southwestern, and we and others have been doing a lot of sequencing, both from patients within our health system, as well as working with Dallas County to help determine which variants are circulating in North Texas. This can give us an idea of what we're facing as a community, and what may be emerging in the near future.

As part of our ongoing commitment to an equitable, effective, and efficient vaccination rollout, UT Southwestern offers a convenient online portal where Texans can sign up to receive a COVID-19 vaccine.
Will the vaccines protect people against the variants?
The vaccines should be effective against these variants. The vaccines are designed to target our immune system and generate antibodies against multiple spots in the spike protein of the coronavirus. So, one change isn't going to dramatically change the efficacy of the vaccine. You would have to have multiple changes. The data so far have shown that these vaccines are already protecting us against the viruses, and while there may be a slight diminishment of how well they protect, in terms of the overall quantity, there's still plenty of protection to fend off serious COVID-19 illness. These comments relate to the two mRNA vaccines that are currently being widely used in the U.S. Some vaccines there is either not enough data or there are potential problems with giving full protection for certain variants.
Will vaccines require a booster to enhance effectiveness?
A year out, a lot of the patients that got infected early on still have robust immune responses, but classically coronaviruses are like common cold viruses – your immune response doesn't last long, maybe a year or two. So, a booster might be needed. Several vaccine manufacturers are already working on creating a booster if necessary, but we're still relatively early in this process and we don't know how durable immunity will be. A third shot is kind of a hedge in that case.
Will these variants prolong the pandemic?
Over the next few months, we need to stay ahead of any emerging variants and try to keep vaccinating the broader community at a brisk pace. Vaccine supply has increased, and I think that bodes well for all of us. That brings up a couple of really important points, which is first, once a vaccine is available to you, absolutely you should get it. The emergence of these variants should not give you pause about waiting for something different down the road.
We feel confident the (current) vaccines will offer robust protection against the current variants.
Second, we need to continue doing the things that protect us from getting and spreading the virus in our own community: social distancing, limiting exposure, wearing a mask, and washing hands. All of those mitigation measures continue to apply, particularly in public places, so as the variants emerge we can keep them from spreading and creating a new surge of cases.
What will see over the next six months in the pandemic?
If the vast majority of people get vaccinated, I think that will go a long way toward ending this pandemic by late summer. Now, the coronavirus may continue to be with us and, long-term it may necessitate the occasional booster shot. But if we all get vaccinated, then I think we will be returning more toward a pre-pandemic life by the end of summer or early fall if vaccine rollout and production continues to go the way we hope.
Tracking the variants
Dr. David Greenberg, an infectious diseases specialist at UT Southwestern, and Dr. Vineet Menachery, a virologist at UT Medical Branch at Galveston, are tracking the COVID-19 variants – and the vaccines’ response to them. In the Jan. 29 episode of "What to Know," they discuss the variants' impact on the pandemic.