Lung transplant: The harrowing journey from donor to recipient
December 13, 2017

This scene has played out in many TV shows and movies: A doctor races through a hospital and into an operating room with a cooler in hand. The cooler is opened and the lungs inside – or the heart, liver, or kidneys – are lifted out and transplanted into the patient lying on the operating table.
While I may not normally run through the hospital, that doesn’t mean the situation is any less dramatic in real life. An organ’s journey from donor to recipient is a well-choreographed process in which there are many players and many steps that must be taken in a precise order.
It all starts with one of the greatest deeds a person can do: organ donation. Donors and their families are heroes. As of December 2017, there were more than 115,000 people on the waiting list for a lifesaving organ transplant, including 122 in Texas waiting for lungs, as of this writing.
Follow me through the lungs’ journey from donor to recipient, a trek that includes advanced medical procedures, ordinary coolers, and unexpected barriers ranging from cancer to tornadoes.
‘We have a lung for your patient’
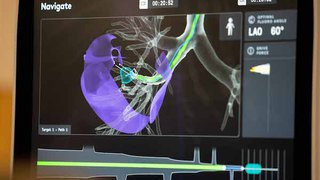
Once a family has given consent to donate a loved one’s organs, the local organ procurement organization is contacted. These nonprofits are responsible for the evaluation of the donor’s organs. For the lungs, this includes a chest X-ray, bronchoscopy, and blood gases.
If these tests show the lungs are suitable for donation, the transplant team of the best-matched patient receives a notification. We have one hour to accept or refuse the offer. During this time, we evaluate the tests that were performed, the donor’s blood type, and the size of the organ to determine if it’s a good match for our patient. If we think it is, we’ll call the patient to inquire about his or her health that day and whether he or she can get to the hospital within a couple hours.
Between the time of death and a transplant team accepting or rejecting an offer, the process can take anywhere from eight to 24 hours. That may seem like a long time, but there’s a lot to coordinate when you’re evaluating multiple organs and contacting the multiple transplant teams and patients who will get those organs.
Communication is key. From the moment I get word an organ may be available to the time we transplant the organ, I may make or receive as many as 50 phone calls, emails, and texts.
Traveling to procure the organs
Once we say yes to the lungs, we call our local organ procurement agency to arrange transportation for the organ. This can include ambulance, helicopter, or airplane, depending on the distance. Surgeons who will procure the donor’s other organs will be making similar arrangements, and it can take four to 12 hours for everyone to get to the donor’s hospital.
We evaluate the lungs again once they’re removed. If they pass approval, they are placed inside three sterile bags and put on ice in a cooler, where they’re kept between 0 and 4 degrees Celsius. And yes, it’s true we use old-fashioned ice cubes and coolers you can buy in your neighborhood store.
Meanwhile back in Dallas, our patient will have made his or her way to UT Southwestern Medical Center. Once we give the thumbs up that the lungs look good and we’re on our way home, the surgical team will begin to prep the patient for surgery.
The return journey and transplanting the lungs
This is when the adrenaline really starts to kick in. We generally want to get the lungs from the donor to the recipient in six hours or less. That’s why we limit travel to a radius of 750 miles, although we do extend this in certain circumstances. For example, in spring 2017, we traveled to Los Angeles to pick up lungs, and the journey took 10 hours – but the patient is doing beautifully.
Weather’s a concern during any trip, and we’ve seen our fair share of bad weather while transporting organs. Once while flying to Dallas with two organs from Wichita, Kan., tornadoes forced us to land in Wichita Falls, Texas. We sped 100 mph by ambulance through driving rain for the remaining 150 miles to Dallas.
When we get to the operating room, the patient will already be anesthetized with his or her chest opened. We’ll examine the lungs once more to ensure they’re still suitable for transplant. Then we’ll remove the patient’s lungs and place the new ones.
When a lung donation falls through
Unfortunately, there are times when the organ transplant journey is cut short.
Only about 30 percent of potential donor lungs meet transplant criteria in the first place. But of the donor lungs that are offered, we end up rejecting or being unable to use 10 to 15 percent of them once we arrive at the surgery to procure organs. This can happen for a few reasons:
- The organ was not as advertised. This could be because of something that was not detected in the earlier tests.
- The lungs have deteriorated since the tests were performed. The lungs are the most finicky of organs and can turn unusable quickly.
- Cancer or a transmissible infectious disease is found in the body. We never want to transfer diseased cells to a patient, so if cancer or transmissible infection is found anywhere in the body, no organs are considered usable. I experienced this not long ago when, after procuring the lungs, the surgeon procuring the kidneys discovered cancer. Despite the lungs looking perfect, we had to cancel the transplant.
It’s disheartening to have to tell a patient who’s expecting an organ that he or she isn’t getting it after all. I’ll usually hold the patient’s hand and say, “I have very bad news. The lungs were just not suitable.” I’ll then explain exactly what we found and why it wouldn’t be a good organ for them. We always prep patients for this possibility, but it’s still frustrating and upsetting for everyone involved.
Organ transplants are one of the most challenging, but rewarding, procedures we perform. There’s nothing better than seeing a patient who was once too ill to participate in daily activities go on to live life fully. No wonder transplant stories make for such good TV!
Want more health stories, information, and tips delivered straight to your inbox? Join our mailing list.