What Texans need to know about mpox
December 5, 2024

In May 2022, there was an unprecedented outbreak of mpox in many countries with no prior history of the viral disease. The international health community swiftly mobilized to deploy tests, vaccines, and therapeutics to contain the outbreak.
More than two years later, cases of mpox continue to emerge, though at a much slower pace. According to the WHO, between January, 1, 2022, and October 31, 2024, more than 115,101 cases and 255 deaths have been confirmed in 126 countries. Just in 2024, there have been more than 21,400 cases globally, with more than 3,000 of those in the United States. according to the Centers for Disease Control and Prevention (CDC).
Though the virus that causes mpox is not novel, we have not seen person-to-person spread at this scale in the past.
If exposed, an overwhelming majority of patients will develop only mild symptoms, which can include:
- Development of “poxes,” blister-like skin lesions
- Swollen lymph nodes
- Genital or oral mucosal lesions
- Fatigue
- Fever
- Sore throat
- Chills
- Headache
- Muscle aches
- Itching
Over the course of the infection, the rash will change from flat patches to bumps and then to fluid-filled lesions that scab over. When the rash and sores break out, the patient is contagious. They remain contagious until all lesions have crusted over, the scabs have fallen off, and a fresh layer of skin has formed underneath.
Most patients with mpox will fully recover at home without medical treatment. Some people may benefit from supportive care to help with fever, pain, itching and care of skin lesions.
UT Southwestern is among the sites across the nation participating in a phase three clinical trial sponsored by the National Institute of Allergy and Infectious Diseases, which is part of the National Institutes of Health. The trial is testing the effectiveness of the antiviral drug tecovirimat in treating mpox. Tecovirimat is an FDA-approved treatment for smallpox.
While the threat to the general population in the U.S. remains low, the COVID-19 pandemic taught us that cautious optimism must be balanced with appropriate precautions. Understanding how mpox spreads and what to do if you are exposed is a good first step in containing the outbreak.
What is the history of mpox?
Mpox, formerly known as monkeypox, is a disease that is caused by the monkeypox virus (MPXV). MPXV is a member of the orthopoxvirus genus. Smallpox, which was eradicated in 1980, belongs to the same genus.
MPXV was first identified in 1958 in Denmark due to an outbreak among laboratory monkeys. The first human case was detected in a 9-month-old boy in the Democratic Republic of the Congo in 1970.
Prior to 2022, the most recent notable outbreak of mpox in the U.S. occurred in 2003 and was limited to 47 cases in six Midwest states linked to animals imported from Ghana to Texas and then to Illinois to be exotic pets.
There are 2 types, or clades, of MPXV: clade I and clade II. The recent U.S. outbreak is from clade II, which continues to circulate in this country at low levels. In mid November, the CDC confirmed the first known case of clade I mpox in the U.S. in a person who had traveled from an area within Central and Eastern Africa, where there are two active outbreaks. The Director General of the World Health Organization declared a public health emergency of international concern for that portion of Africa in August 2024 that remains in effect.

How does mpox spread?
Mpox is mainly spread from person to person through close contact. This includes but is not limited to sexual contact. Transmission occurs through exposure to bodily fluids, lesions on the skin or mucosal surfaces such as the mouth and throat, respiratory particles, and contaminated objects. MPXV is also found in small mammals in tropical rainforests in central, east and west Africa, and exposure to infected animals can lead to infection in humans.
Because the virus is not novel, we have a basic understanding of the disease progression of mpox and how to contain the spread. Infections typically last two to four weeks, and symptoms generally begin one to two weeks after exposure. Mild symptoms such as fever and fatigue may come first, followed by skin lesions that flare up, scab over, and fall off without intervention. People remain contagious until those scabs fall off to reveal a new layer of skin underneath. It’s also worth noting that not all cases have had fever before the rash.
About 99% of patients with the clade II mpox make a full recovery, though in severe cases infection can be fatal. Patients with severe cases are being treated with tecovirimat. Its effectiveness is still being studied.
The CDC recently reported a cluster of cases in the U.S., dating from Oct. 6, 2023, to Feb. 15, 2024, that showed resistance to tecovirimat: five cases in California, eight in Illinois, two each in Louisiana and Texas, and one in New York. While health officials were aware of resistance developing among patients who were previously treated with the drug, the 18 patients in this cluster had no treatment history.
Who is at risk of contracting mpox?
Anyone exposed to the virus can be infected. People who are at increased risk include:
- Those with immunocompromising conditions such as cancer or HIV/AIDS
- Gay and bisexual men, who comprise many of the current U.S. cases, according to the CDC, though the agency emphasized that anyone can contract mpox through close personal contact regardless of sexual orientation
- Individuals who have been bitten by or exposed to a live or dead infected animal
- People who are pregnant
- Children
What should you do if you are exposed to mpox?
If you don’t feel well, stay home, and avoid close contact with others, especially if you have an unusual rash. Call your doctor if you have symptoms and discuss your next steps.
Currently, people in the U.S. with mpox are advised to isolate at home until symptoms resolve. If people with mpox have to be around other people, they should cover all of their lesions. Most patients will recover without medical intervention. In severe cases, patients may require hospitalization and medications for the infection and complications.
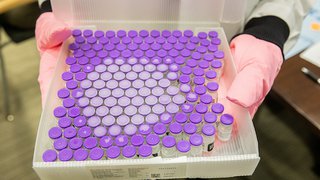
Is there a vaccine to reduce your risk of getting mpox?
There is an available mpox vaccine, the JYNNEOS vaccine, that is effective against mpox and smallpox. The CDC recommends this mpox vaccination for those who have increased risk of acquiring mpox. This vaccine is also recommended to prevent infection in people with exposure to someone with mpox in the last 2 weeks. Contact your doctor or the health department as soon as possible if this applies to you.
People planning to travel to Central and Eastern Africa [VW1] should follow the CDC’s travel notice information to protect themselves and others. Talk with your doctor about whether you need to be vaccinated.
Just as we’ve been doing the last few years, make sure to follow basic self-protection guidelines: Wash your hands regularly, pay attention to potentially suspicious symptoms, and keep your distance from others if you are experiencing even mild symptoms.
To talk with an expert about mpox or to learn more about the clinical trial, call 214-645-8300 or request an appointment online.