The Peter O’Donnell Jr. Brain Institute brings together transformative research and patient-centered care to improve the lives of patients today and those of generations to come.
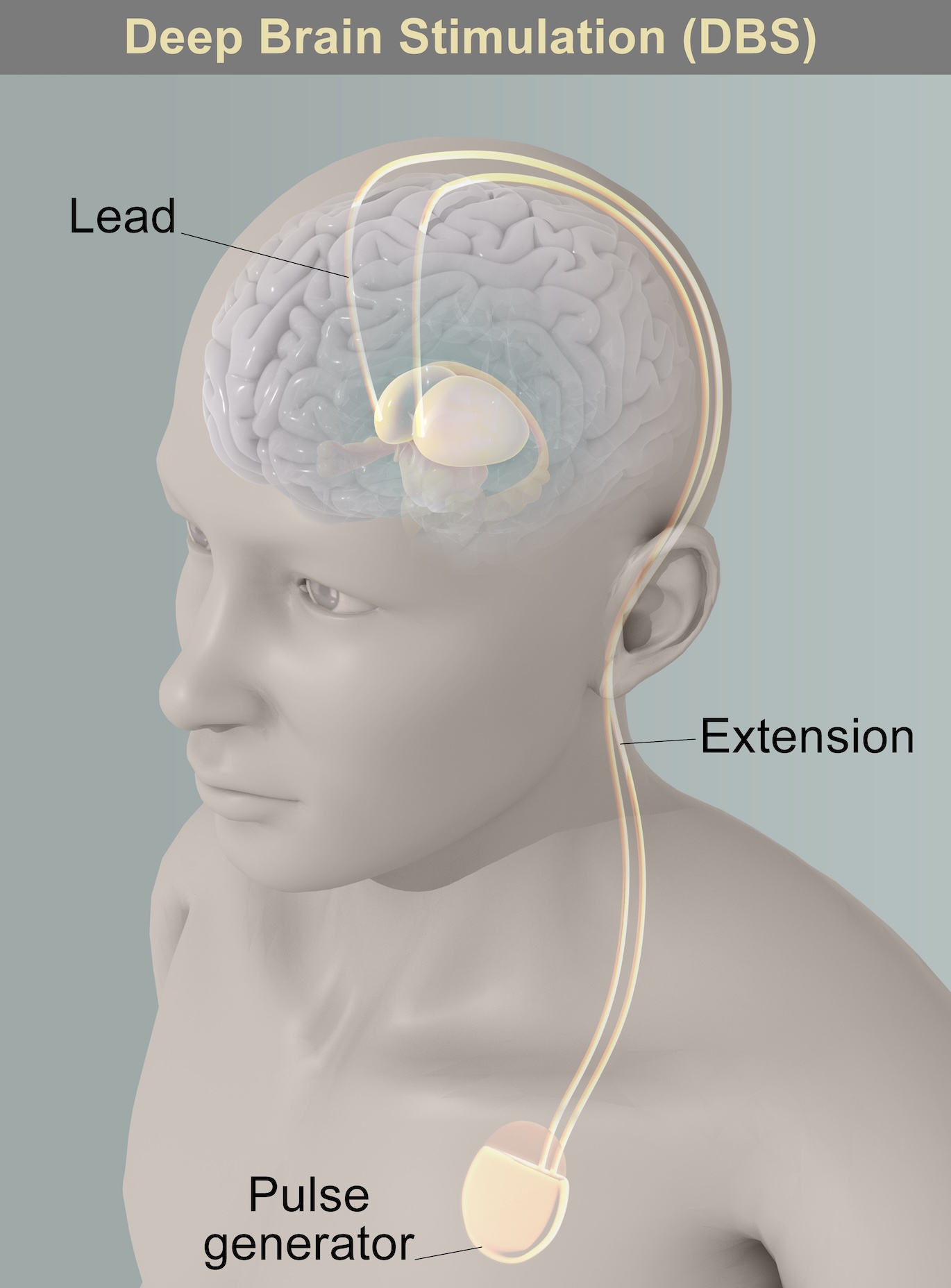
For patients with Parkinson’s disease, DBS is intended to provide more consistent control of motor symptoms.
The symptoms that can be managed with deep brain stimulation include:
- Rigidity (or stiffness)
- Bradykinesia (or slowness)
- Tremor
- Dyskinesias
- Dystonias
DBS is most often recommended for patients with:
- Motor fluctuations
- Disabling off periods
- Disabling dyskinesias
- Unpredictable response to medications
- Dystonias
- Medication-refractory tremor
DBS does not improve balance issues, speech issues, cognitive function, autonomic dysfunction, and swallowing function.
DBS is not meant to be a substitute or replacement for medications. Rather, it works as an adjunctive therapy to make the medications work more consistently.
In general, patients should expect to spend more time with the best symptom control they can achieve with medications. Response to medications for Parkinson’s disease is one of the best predictors of how someone will benefit from deep brain stimulation. The one motor symptom that can respond to deep brain stimulation that does not get better with medications in tremor.
Two common targets for deep brain stimulation in Parkinson's disease are the subthalamic nucleus (STN) and the globus pallidus interna (GPi).