
It’s not uncommon for a patient to tell their health care provider, “I have a hemorrhoid.”
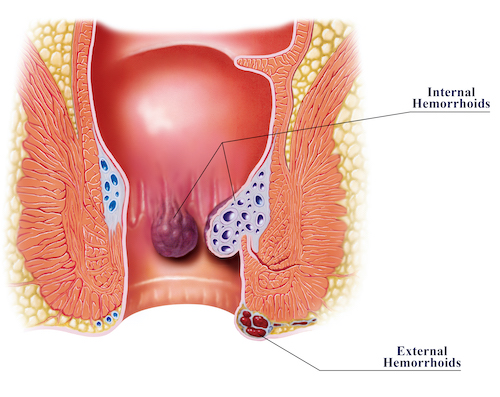
But that statement can be interpreted in many ways, because we’re all born with hemorrhoids. In their natural state, hemorrhoids are the vascular structure in place at the bottom of the anal canal.
A more accurate description for what the patient is experiencing is “symptomatic hemorrhoids.”
Internal hemorrhoids are the body’s natural way to cushion stool until one is ready to defecate. Within the anal canal, there are three columns of hemorrhoids to assist the body with holding stool before defecating. Internal hemorrhoids do not contain nerve endings because they are above the dentate line, a line that divides the upper two thirds and lower third of the anal canal. But they can become swollen and cause uncomfortably and sometimes painful symptoms. Swelling can be caused by:
- Excessive straining
- Hard, formed stools
- Sitting on the toilet for long periods of time (more than five minutes)
- Lack of water intake
- Lack of physical activity
- Lack of fiber
- Adequate fiber intake but with lack of water intake
- Pregnancy
- Diarrhea
Chronic or repeated swelling of internal hemorrhoids is classified as hemorrhoidal disease, and symptoms include anal itching, painless bright red bleeding, prolapsing or bulging of the hemorrhoidal tissue, and pain due to thrombosis or a blood clot.
Measuring hemorrhoid disease
Internal hemorrhoidal disease affects about 10 million people per year in the United States, or about 4.4 percent of the population, according to recent studies. It is typically diagnosed during an anoscope exam, which is performed in the doctor’s office, or via colonoscopy, which is performed in a procedure room under light sedation. Internal hemorrhoids are categorized by a grading system that measures the degree to which they prolapse from the anal canal.
- Grade 1 hemorrhoids may bulge slightly into the anal canal but do not fall below the dentate line.
- Grade 2 internal hemorrhoids swell and prolapse out of the anal canal, filling half the anoscope, a two-inch wide hollow tube equipped with a light that allows the provider to examine the anus and rectum. Grade 2 hemorrhoids reduce spontaneously.
- Grade 3 internal hemorrhoids fill the anoscope and prolapse outside of the anal canal while straining or defecating. Manual reduction is required. This means the hemorrhoids fall below the dentate line and pain may be present.
- Grade 4 internal hemorrhoids are severe, irreducible, and have the potential to strangulate, which can cause extreme pain.
If hemorrhoids develop below the dentate line, they are considered external hemorrhoids and are in place to communicate with the internal hemorrhoids and drain into the veins in the pelvic area, and then ultimately the inferior vena cava leading to the heart. They become swollen and possibly thrombosed with the same causes of swollen internal hemorrhoids. The nerve endings meet below the dentate line, causing the pain receptors to flare.
Conservative treatments for hemorrhoidal disease
Studies have shown that more than 80 percent of patients will require no surgical intervention for hemorrhoidal disease (internal or external) if conservative measures are followed appropriately, which is why we begin there.
1. Typically, the first step is to measure fiber intake.
Does the patient get 20 to 30 grams of fiber per day? Fiber is needed to bind the stool, bulk it up, and soften it. Foods rich in fiber include avocados, beans, fruits (apples, bananas, and pears), and vegetables (peas, broccoli). If the patient does not get enough fiber, it is important to consider dietary changes and add a supplement. Not all fiber supplements work the same, so it is important try different brands or types. For example, Metamucil gets mixed with a full glass of water and requires eight additional glasses of water a day. If the patient is not a regular water drinker, fiber gummies are a good alternative. The goal is for a patient to have a soft, easy-to-pass stool (equivalent in consistency to toothpaste). Patients can start with one fiber gummy a day and work up to five safely to achieve the desired outcome. Benefiber, another viable option, can be mixed with other foods such as mashed potatoes or even soup.
As mentioned before, fiber without enough water may cause constipation, so consider the patient’s medical history and fluid volume. Fiber supplements can also cause a patient to bloat and have increased gas, but these symptoms tend to subside after a week of therapy while the body adjusts to it.
2. Avoid straining while defecating and sitting on the toilet for more than five minutes.
This can increase swelling and aggravate symptoms of internal hemorrhoids. If patients are not able to defecate within five minutes, get up and try again later when ready. Thirty minutes of cardiovascular exercise per day is recommended to stimulate gut function. It takes an average of three months to see results with conservative measures, but improvements may be noticeable after one month, such as reduced bleeding.
Surgical approaches for hemorrhoids
If a patient’s condition does not improve with conservative lifestyle modifications such as fiber, water, and exercise, then surgical approaches may be considered. The most common procedures are rubber band ligation and a conventional hemorrhoidectomy.
Rubber band ligation can be performed during a colonoscopy or in the clinic setting and is the most common approach for symptomatic grade 2 or grade 3 bleeding internal hemorrhoids. It is an easy, inexpensive procedure to perform and complications are rare.
The procedure is not recommended for patients on blood-thinners (excluding low-dose aspirin), with cirrhosis of the liver, or hypertension due to increased risks of delayed-onset hemorrhaging. This procedure is performed by a colorectal surgeon, who uses an anoscope to place a small rubber band ring on the base of the internal hemorrhoid. The patient will feel pressure for about 24 hours but the internal hemorrhoid will strangulate and eventually pass through the anal canal. Patients can return to work the next day, but they should monitor for bleeding and avoid travel for two weeks after the procedure. If severe blood loss should occur, call emergency medical services. Rubber band ligation cannot be performed on external hemorrhoids or external skin tags because these fall below the dentate line and would cause severe pain.
Conventional hemorrhoidectomy is the second common surgical approach, and it can be performed through a minimally invasive technique that has a 95 percent success rate. The goal of the surgery is to remove repeatedly swollen tissue, while avoiding any damage to the anal sphincter or removing too much of the anoderm, which could lead to anal stenosis.
Complications may include urinary retention, urinary tract infection, post-operative bleeding, fecal incontinence, and/or anal stricture. The most common reason to avoid hemorrhoidectomies is the post-operative pain, which typically lasts two weeks. Surgeons may administer nerve blocks, but they are unlikely to alleviate all pain during recovery.
Following this procedure, patients take stool softeners to prevent constipation until their bowel habits have returned to normal as well as their pain control and eating habits. If the underlying cause of hemorrhoidal disease is not addressed, the internal hemorrhoids are likely to return with the same symptomatic problems within several months.
Misconceptions about hemorrhoidal disease treatments
1. Stool softeners and stimulants won’t fix the problem.
Commonly prescribed stool softeners, such as Docusate (Colace) and Sennosides (Senna), are often prescribed to help with constipation. They draw more water into the colon, making stool easier to pass through the anal canal. While that may seem helpful, stool softeners don’t increase the frequency of stools and, therefore, don’t fix the patient’s underlying problems. Stool softeners are useful for patients recovering post-operatively due to lack of activity, hydration, and stimulation of the bowel.
Polyethylene glycol/Miralax, an osmotic bowel stimulant, is also a commonly used medication for constipation. It can cause diarrhea, which is one of the irritants and causes of symptomatic internal hemorrhoids. Miralax is best prescribed when the patient has attempted a fiber supplement and needs an additional bowel stimulant with it. It should be used primarily with colonic inertia (slow transit constipation).
2. Removing a hemorrhoid isn’t always the best option.
Colorectal surgeons won’t automatically remove a thrombosed hemorrhoid, particularly when a blood clot is present on the external portion of the anus. Patients can usually tolerate the pain with some assistance from over-the-counter medication, sitz baths, witch hazel wipes, and other measures. Pain will likely increase suddenly and slowly decrease after three to five days until it has resolved in two weeks. By the time a patient sees a colorectal surgeon, they are typically over the peak of pain. If patients are starting to slowly improve, the benefit versus risk of surgery is weighed, and conservative measures will likely be recommended.
3. A hemorrhoidal skin tag may not need to be removed.
Some patients inquire about having external skin tags, or extra skin present on the anus from a previous external hemorrhoid, surgically removed. But skin tags usually don’t cause pain and removing it is purely cosmetic. It can also make it difficult for the patient to clean the area.
Clearing up confusion about hemorrhoidal disease
Hemorrhoidal disease is a topic many people will have to address at some point in their lives. Conservative management may be the most powerful tool to treat symptomatic internal hemorrhoids. Management includes keeping stools soft through fiber rich foods, a fiber supplement, avoiding straining while defecating, not sitting on the commode more than five minutes at a time, increasing physical activity, and drinking 64 oz of water per day or more (with consideration of medical history).
After three months of conservative measures, if the patient is continuing to experience hemorrhoidal disease symptoms, it could be time to consider rubber band ligation or a hemorrhoidectomy.
If you have questions about hemorrhoidal disease or would like to speak with a colorectal specialist, please call 214-645-8300 or request and appointment online.










