Almost exactly a year ago, I was interviewed on the subject of “superbugs” and the potential for bacterial and viral infections to spread quickly across the world. A 60 Minutes report had delved into the topic, specifically focusing on growing concerns about antibiotic-resistant bacteria. But many of the underlying conditions that made us susceptible to the spread of the novel coronavirus, COVID-19, are the same.
We live in an incredibly interconnected world, where it is possible to travel from one continent to another within hours, potentially carrying and spreading unknown or new pathogens along way.
SARS-CoV-2, the virus that causes COVID-19, originated in an animal market in Wuhan, China, in late 2019. Less than six months later, more than 3 million cases have been confirmed worldwide – in nearly every country, including more than 1.1 million cases in the U.S.
A global pandemic is frequently on the short list of nightmare scenarios for epidemiologists, health care providers and others involved in public health. They keep us awake at night and working long hours in the lab, largely because we understand the damaging health and societal effects a pandemic can have on communities. In some ways, COVID-19 feels as if it has been around for an eternity; it has fundamentally altered our daily lives – how we work and play, eat and learn, shop and worship.
But in the life cycle of a never-before-seen virus, six months is a blink of an eye. That’s why many questions remain about COVID-19, such as:
- When will we find treatments that improve outcomes in patients who are infected by this virus?
- Will COVID-19 be a single (albeit large) event, similar to SARS and MERS or will it become a mutating seasonal virus like influenza?
- If and when we develop a vaccine, will it be a universal vaccine similar to the one for measles, or will it be an annual shot such as with influenza?
- Will the antibodies patients develop protect them from future COVID-19 infection?
The good news is that the world’s scientific and medical communities, including many of us at UT Southwestern, have rallied together to conduct clinical trials and research, and collect data in real time. We are actively sharing discoveries in hopes of creating a global game plan to combat, and eventually eradicate, COVID-19.
COVID-19 and treatments: How they might work
Viruses have been around a long time – 3.5 billion years by some estimates – which means they have become very resourceful. Mostly made up of strands of DNA or RNA wrapped in a soft protein shell, viruses slip inside a host – people, plants, or animals – and invade healthy cells, coaxing them to make copies of the viral genetic material and multiply.
COVID-19 is a respiratory virus that is released through tiny droplets when we breathe, talk, cough, or sneeze. It is easily spread from one person to another, either by inhaling the droplets or touching a contaminated surface and then touching our eyes or nose. Without a host, however, the virus cannot survive, which is why physical distancing and travel restrictions remain vital to limiting the spread and squelching the pandemic.
UT Southwestern has participated in several of the country’s most robust and promising clinical trials to explore whether existing drugs can effectively treat COVID-19. The therapies follow two distinct paths: antiviral drugs that attack the infection and try to “kill the virus”; and inhibitors that treat the host, trying to keep our own immune response from getting too out of control.
The COVID-19 Trials
Dr. James “Brad” Cutrell, Medical Director of Antimicrobial Stewardship at Clements University Hospital, joins our host, Dr. John Warner, Executive Vice President for Health System Affairs, to provide an inside perspective on clinical trials and the search for coronavirus therapies.
Remdesivir: Breaking the RNA chain
Remdesivir, an antiviral, intravenous drug developed after the Ebola outbreak in 2014, has been the focus of multiple clinical trials, including a large scale, randomized trial led by the National Institute of Allergy and Infectious Diseases including more than 1,000 patients at 100 medical centers.
Remdesivir blocks the protein COVID-19 uses to make copies of its RNA genetic material, and recent results demonstrated that recovery time for hospitalized patients who received the study drug was reduced from an average of 15 days to 11. Based on the interim results, the FDA announced on May 1 that it has approved the emergency use of remdesivir to treat COVID-19 patients. UT Southwestern is currently involved in other clinical trials studying remdesivir.
Sarilumab: Calming the immune system storm
Sarilumab, a drug that employs a monoclonal antibody to combat interleukin 6 (IL-6), a cytokine that causes inflammation in COVID-19 patients, was the focus of another clinical trial at UT Southwestern. When our body’s immune system senses the presence of a virus, it naturally triggers a response aimed at neutralizing the infection. Sometimes this immune response can lead to excessive inflammation and this drug attempts to target this side of the equation.
Sarilumab, which may mitigate that exaggerated response, has already received approval from the FDA for treatment of rheumatologic disease. But its use for COVID-19 is still pending clinical trial results.
Nearly 50 percent of the COVID-19 patients who were treated at UT Southwestern’s William P. Clements Jr. University Hospital were enrolled in one of our clinical trials, led by my colleague Dr. Mamta Jain and involving a large group from UT Southwestern’s Infectious Diseases and Geographic Medicine Department and other areas of the hospital system. The clinical trials represent the gold standard for developing effective treatments. We would not be able to push forward with COVID-19 discoveries without the dedication of these providers and the extraordinary commitment of our patients.
'Optimistically, the goal for COVID-19 would be to create a vaccine that produces a durable set of protective antibodies that would eliminate the pathogen entirely, now and in the future. Among the many unknowns about this coronavirus is if it will mutate enough in the future to become a seasonal part of our lives.'
David Greenberg, M.D.
What will it take to create a vaccine?
Existing drugs like remdesivir and sarilumab may help reduce the suffering of COVID-19 patients and provide incremental benefit in the effort to weaken the pandemic. Eliminating the disease, however, is another story.
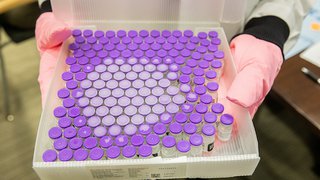
Six COVID-19 vaccines are being tested in phase 1 clinical trials, and we will be watching those very closely. But in reality, the earliest a vaccine will likely be available is next spring or summer, because of the extensive safety testing required.
Among the many unanswered questions about a vaccine is whether it will be the “Holy Grail” variety, a one-time, universal prevention much like the measles or HPV vaccine. Or will it resemble the annual flu vaccine?
Some respiratory viruses, like influenza, mutate just enough each year that they become seasonal and infectious disease experts work to investigate and anticipate the new strain to develop an effective vaccine.
Optimistically, the goal for COVID-19 would be to create a vaccine that produces a durable set of protective antibodies that would eliminate the pathogen entirely, now and in the future. However, among the many unknowns about this coronavirus is how it will behave in the future – and if it will mutate enough to become a seasonal part of our lives.
Antibody testing – it’s complicated
Antibody testing has become a hot topic in the daily download of media coverage, and some outlets have hailed these serological tests, which can identify past infections, as a magic bullet to ending the COVID-19 crisis and re-opening society.
Linking those two notions is based on an assumption that if you have antibodies, you are protected from being infected by the virus – though honestly, it has not been proven that this is the case with COVID-19 as of yet. Also, the accuracy of antibody testing kits is murky at best. Researchers in California reviewed 14 antibody tests on the market and found only three produced consistent results.
What is clear is that every day we are bombarded by viruses and bacteria, and our immune system does a pretty good job of recognizing these foreign objects in the body and developing the appropriate response. That includes producing antibodies, or blood proteins, which are created specifically to counteract a pathogen. But just because we make antibodies does not automatically mean they’ll be powerful enough to prevent an infection.
The real value of antibody testing is to better understand just how many people have been infected. It’s very possible that many people are asymptomatic and spreading the virus without knowing it. Serological testing can provide clues to the full scope of the pandemic.
Convalescent plasma shows promise
Antibodies play a role in another potential treatment for COVID-19.
Convalescent plasma is a therapy that has been around for more than 100 years. It involves taking plasma from a patient who has survived a viral infection and had an immune response and then injecting the purified antibodies into a patient who is actively fighting the same infection. We have treated about 10 COVID-19 patients at Clements University Hospital in the last few weeks with convalescent plasma, and we are hopeful it will produce positive results, as it did in two very small studies recorded in China.
Convalescent plasma was used to help manage viral infections during the 1918 influenza pandemic and the Ebola outbreak in 2014, and it has been approved by the FDA for emergency use for COVID-19. Blood donation centers around the country are also taking plasma donations from recovered COVID-19 patients in hopes it will provide another therapeutic option against the novel coronavirus.
A worldwide solution is what we need
COVID-19 has taught us many things in a relatively short period of time, from the importance of hand hygiene and social distancing to just how much we value our families and freedom to move about the world.
No country, city, or region is immune from the spread of a viral infection, particularly one we’ve never seen before, and that should be a common thread that binds us together.
This really is a global problem, and it will require global solutions.
As our populations grow, we will remain at risk for future pandemics. Reducing that risk will require an unprecedented level of collaboration from the scientific and medical communities, which we have already seen in the last few months.
It will also require significant investment in basic science and public health – a relatively small price to pay to escape the economic and human impact of another COVID-19 crisis. Working together, we will get to the other side of this pandemic, and I hope we will apply the valuable lessons we learn from COVID-19 to improving the future of health care for all humanity.