I’m a cardiologist who has a special interest in sports and exercise training. Part of the reason for that is because as an undergraduate at Brown University, I played tennis and wrestled. I know how hard athletes work, and I understand how dedicated they often are to their sports.
I also empathize with how it can crush athletes when their doctors suspend them from practice or competition, even for just a few weeks. There’s fear of losing their competitive edge, muscle mass, and chances at scholarships.
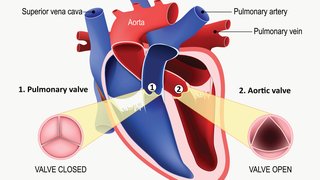
Now imagine if results from a pre-participation electrocardiogram (ECG, also known as an EKG) suggest you may have a heart condition that you didn’t know about, and because of that your doctor says you can never play your sport again or, even worse, that your condition is fatal.
That’s the situation many of my patients face. Athletes are referred to me after they’ve been given vague or serious news about their heart health. We expect to see more of these patients with the advent of the 2016 NCAA recommendations about whether all student-athletes should undergo pre-participation ECG screenings for arrhythmias and heart disease.
What do the 2016 NCAA guidelines say about ECG screening?
To create the 2016 recommendations, the NCAA appointed a task force to address concerns about sudden cardiac death in college student-athletes. I’ve been involved in creating national guidelines (called the Bethesda Conference Guidelines) since the early 1990s, along with many other experts from around the country. One of these experts is world-renowned electrophysiologist Mark Link, M.D., who will join our team in Dallas in fall 2016 as Director of Cardiac Electrophysiology.
The task force addressed three controversial points:
- The purpose of pre-participation ECG screenings
- Best practices for screenings and interpretation of findings
- How institutions should plan for and handle cardiac emergencies
Screening all athletes sounds like a solid plan that would help prevent death. However, there are five factors to consider when deciding whether to intensify screening of athletes with an ECG:
- Sports cardiology specialists are vital in caring for athletes and interpreting ECG findings, family histories, and physicals because they understand the risks of a suspected cardiovascular disease.
- It is not proven that ECG screening will prevent athlete sudden cardiac death.
- Pre-participation ECGs may increase false alarms for some athletes.
- Sports may not worsen all conditions, and we can’t prevent all deaths. Identification of an inherited cardiac condition is not the same as saving a life, as many of these individuals will/would live a long life.
- Teaching resuscitation (AED and CPR) is not emphasized enough in high schools, colleges, and coaching/training programs.
Although the new NCAA recommendations are noteworthy in their desire to reduce death in athletes, there are many issues which will arise in their implementation.
1. Sports cardiology specialists are vital in caring for athletes
The 2016 cardiac care guidelines recommend the development of regional referral centers for sports cardiology. That’s what we’re building here in Dallas. For the past 24 years, I’ve directed the Dallas-based Institute for Exercise and Environmental Medicine (IEEM), a partnership between UT Southwestern and Texas Health Presbyterian Hospital Dallas. I’ve worked with athletes from all over the country who have unique cardiovascular conditions, from high school athletes to professionals. My team’s goal is to get these athletes back in the game safely — and often, we can.
Now we’re focusing on developing the IEEM into a regional center of excellence. We see cases every day that most cardiologists see only once or twice a year. It’s difficult to decide how to manage these cases, and nonspecialized cardiologists may feel more comfortable erring on the side of caution and keeping these athletes out of sports. The IEEM provides these doctors a referral center for extensive testing to determine whether it’s safe for athletes to continue their sports.
Part of our job is to explain to athletes and their families what we know and don’t know about their conditions, including risks and benefits of continuing in their sports. As with any health concern, such shared decisions are made by being honest with athletes and their families, and together weighing risks and benefits, not by “preventing” or “allowing” sports participation. The decision to return to play is guided by the benefits and risks to the athlete, and the athlete and their family considerations are taken into account. There are times when, even if risks cannot be completely eliminated, there may be methods to allow return to play with appropriate monitoring.
We used this strategy with a young woman who was suspected of having long QT syndrome — an inherited heart condition that can cause life-threatening arrhythmias. She was an Olympic-level athlete who, after a screening test, was told she couldn’t compete in an upcoming national championship. She was then referred to us, and after extensive testing and discussion, we determined that she could compete. She went on to win an Olympic medal.
Now imagine if that athlete and her doctor had taken her original testing at face value rather than referring her to a specialist. She would have missed out on a once-in-a-lifetime opportunity to represent her country in the Olympics, all because of fear of the unknowns about her disease.
2. ECG screening isn’t proven to prevent athlete sudden cardiac death.
There is a widely quoted Italian study which shows the reduction of athletic sudden death with a screening program which includes ECGs. However, this study has never been replicated, which is one of the fundamental tenets of modern medicine. The reason ECG screening works in Italy – and so far only in Italy – may be due to the relatively high prevalence of genetic forms of heart disease in the country.
Israeli and Japanese studies did not confirm the benefits of ECG screening. Also, many diseases that cause sudden death in athletes cannot be detected by ECGs.
3. Pre-participation ECGs may increase false alarms
One of the more hotly contested controversies surrounding the 2016 recommendations is whether all athletes should have an ECG screening before participating in a sport. It’s controversial because there are no good data to support either side of the debate, and emotional considerations often take over the conversation.
One side of the controversy argues that coaches, trainers, and doctors must do everything we can to save a single life, even if it means thousands of student-athletes are kept out of sports. The other side is that doctors can’t eliminate all risk for any heart condition, many of the available therapies are dangerous in their own right, and keeping kids out of sports may do more harm than good in the long run.
We know regular exercise helps prevent challenges such as obesity, Type 2 diabetes, and lifestyle-related heart disease later in life. And we don’t want to create a generation of “cardiac cripples” — people who are afraid to be active, or even walk up flights of stairs, for fear of dropping dead from cardiac arrest.
We are concerned that making ECG screenings mandatory for pre-participation may increase false alarms. ECG screening will identify cardiac abnormalities, some serious and some trivial. Some of these patients will be subjected to additional worry, expenses, and testing, which also can pose risk. Other patients may be labeled with vague or false diagnoses. These gray areas can lead to a lifetime of fear about something that may never happen, or that may happen but not because of exercise. These are complex situations that require specialized care.
Our sports cardiology program focuses on caring for athletes who may have or definitely have cardiovascular disease by:
- Confirming whether an athlete really has a disease
- Determining if there is a need for medication or other treatment
- Deciding with the athlete and family whether the risks of playing a sport outweigh the benefits
- Determining whether family members also should be screened if the disease is genetic
We’re also beginning a research project called the North Texas Pilot Project, which is a randomized study involving eight North Texas high schools. Half of the student-athletes will receive a pre-participation physical and family/personal history evaluation, while the other half will receive both of these plus an ECG screening. We will track and follow participating students’ health as they become college athletes and adults.
Although sudden cardiac deaths in athletes often receive a lot of media attention, these tragedies are rare. To determine whether ECG screenings help prevent cardiac death, we would need to conduct a much larger study, but the North Texas Pilot Project will give us baseline data as a starting point.
4. Sports may not worsen all conditions, and we can’t prevent all deaths
If athletes are passionate about their sports, we’ll exhaust all available testing to help them stay safe while participating. It’s rare that we have to help an athlete understand why participation isn’t a safe choice, though this outcome does happen.
There are strong data that sports can worsen a few select heart conditions, but those are rare:
- Polymorphic VT is absolutely triggered by exercise — cardiac arrests happen only during exercise.
- Long QT is triggered by exercise in roughly one-third of cases.
- Arrhythmogenic right ventricular dysplasia appears to be triggered by exercise and athletes with this condition actually can accelerate the disease process by playing sports.
On the flip side, hypertrophic cardiomyopathy (HCM) is one of the more common heart conditions associated with sudden death, but there are no solid data to suggest that sports triggers HCM. Athletes with HCM are probably as likely to die in their sleep as they are on the court or the field. If a high school athlete dies on the playing field, it makes the news. If that same athlete died in his or her sleep, it likely wouldn’t.
There are two factors that can increase arrhythmias: acute triggers (pressure to succeed and sports-related emotional stress) and long-term effects from worsening of a condition or another underlying disease. To really understand whether sports makes these conditions worse, we need to study more athletes.
When I talk with patients about their conditions, we also discuss the potential consequences of decisions in their care. I tell athletes, “If you want complete safety, take up chess and don’t play your sport anymore.” Doctors can’t prevent all sudden cardiac deaths, even with exceptional monitoring and care.
A personal example
One of my most memorable patients was a high school student who was preparing for a national crew race championship. After a preliminary race, he nearly fainted. His doctors didn’t know what to do, so they referred him to me. We ran extensive cardiac and exercise stress tests and even reproduced a competitive rowing event in my laboratory. When we couldn’t induce even a single abnormal heartbeat in him, I gave him clearance to compete. The young man won the national championship and was offered a full college scholarship for rowing.
A few weeks later, I was at an American College of Sports Medicine meeting when I missed a call from my patient’s father. He left me a voicemail to tell me his son was dead.
My heart began to pound out of my chest. When I called the father back, I sputtered, “I’m so sorry.” He quickly assured me that his son’s heart hadn’t failed — the young man had died in a car accident. The father had called to thank me because we worked with his son to help fulfill his dream of becoming a national rowing champion and scholarship winner. “If you had kept him out of that race,” the father said, “he would have died without having achieved those life dreams.”
5. The importance of teaching resuscitation (AED and CPR)
The 2016 NCAA recommendations place a large emphasis on cardiac resuscitation, and rightly so. Resuscitation training will save more lives than pre-participation ECG screening programs. Even if we detect all known cardiac conditions in athletes, we’ll still see sudden deaths — in athletes or in parents and spectators who have heart attacks in the stands.
Dr. Link is a world expert in commotio cordis — a sudden cardiac death that we can’t screen for. Commotio cordis is sudden death from a blow to the chest. We’ve seen this in players who get hit with a hockey puck, baseball, softball, or basketball. While screening can’t prevent commotio cordis, knowledge of resuscitation techniques will.
It’s mind-boggling that all high schools do not mandate CPR and AED training. There’s a week of sexual education, but not two hours of resuscitation training? But this is changing. As of 2016, 32 states — including Texas — require CPR training for high school graduation. The American Heart Association has set a goal to make resuscitation training mandatory in all 50 states by 2020. We can never prevent all sudden deaths, but the bottom line is the public needs to be better educated on how to perform CPR and AED resuscitation when cardiac emergencies happen.
Who should be screened for heart conditions?
If you’re trying to decide whether you or your child should have a pre-sports heart screening, there are a few things to consider:
- Family history of premature or sudden death. If anyone in your family history died suddenly or prematurely, schedule a pre-participation ECG. For example, I met with an NFL player in April 2016 for a suspected heart condition. I asked whether he had a family history of sudden death, and he told me no. I asked if he had siblings. He did, and his mother had suffered several miscarriages before he was born. We then discussed his parents — they both were healthy. Then his grandparents, one of whom died when the player was a baby. His grandmother had fallen from a farm vehicle, but he wasn’t sure whether she was in a wreck or whether she’d fainted or suffered a heart attack. We called his mother to find out before we moved on to the next steps in his evaluation. It’s vital to cover every scenario and dig deeply and completely into the family history to keep patients safe.
- Personal history of heart disease. If you or your child have an inherited heart condition, have had any type of heart surgery, or have ever suffered a heart attack, get a pre-participation ECG and other related testing your specialist determines is necessary.
- Cardiac symptoms. If you or your child experiences or has experienced cardiac symptoms during or after exercise, get a pre-sports ECG. Common cardiac symptoms include:
- Fainting or near-fainting, particularly during exercise
- Dizziness
- Lightheadedness
- Chest pain or discomfort during exercise
- Palpitations
- Sudden acceleration or deceleration of heart rate
Whether you’re a weekend warrior who enjoys the challenges of marathon training or an elite student-athlete working toward a college or professional sports career, pay close attention to your heart health. Though we can’t prevent all cardiac events, we can help you navigate a complicated diagnosis and balance the risks with the benefits to help you enjoy a safe and healthy athletic life.
If you’re looking for answers about your or your child’s pre-participation ECG, request an appointment with a sports cardiologist.