Radiation Oncology Clinical Trials Home In on Personalized Treatments
January 22, 2025
Nonsurgical approaches could transform breast and kidney cancer care.
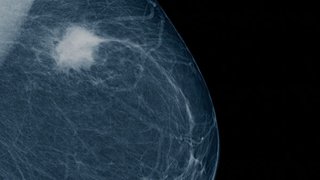
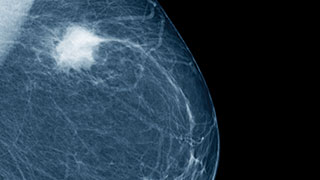
Seeking Alternatives to Breast Cancer Surgery
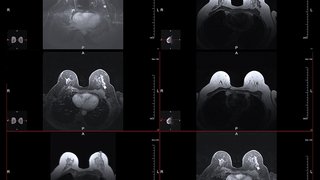
A multiple principal investigator grant from the Cancer Prevention and Research Institute of Texas (CPRIT) will fund a phase II clinical trial evaluating preoperative stereotactic ablative body radiotherapy (SABR) at a single fraction of 30 Gy in patients with early-stage estrogen receptor-positive (ER+) breast cancer.
The trial builds on encouraging preliminary data from an ongoing phase I study that was presented as a late-breaking abstract at the 2023 American Society for Radiation Oncology (ASTRO) Annual Meeting. Asal Rahimi, M.D., M.S., Professor of Radiation Oncology at UT Southwestern, is the study’s co-principal investigator with Basak Dogan, M.D., Professor of Radiology and Director of Breast Imaging Research, and Prasanna Alluri, M.D., Ph.D., Assistant Professor of Radiation Oncology.
According to Dr. Rahimi, surgery stands as the cornerstone of treatment for patients with localized breast cancer. But nonsurgical modalities like SABR could reduce treatment-related side effects while maintaining effective disease control.
“If successful, our study could pave the way for a paradigm shift in treatment by eliminating the need for surgery, providing an alternative option to the current standard-of-care treatment, which is lumpectomy plus sentinel lymph node mapping as well as one to four weeks of breast radiation."
Asal Rahimi, M.D., M.S.
In the upcoming trial, patients will be evaluated for lymph node involvement using a novel nonsurgical approach called microbubble contrast-enhanced ultrasound prior to SABR. Optoacoustic ultrasound imaging will be used to evaluate a patient’s response.
“Two novel imaging modalities seemed like the best fit for this trial,” Dr. Dogan says. “With the assistance of microbubble ultrasound contrast, the patients could potentially avoid surgical sentinel lymph node biopsy. We could noninvasively detect metastatic nodes without the need for radioactive dye injection, general anesthesia, or surgery. Optoacoustic imaging shows the cancers’ oxygenation status and can help us distinguish patients who are most likely to benefit from SABR as well as detect their response after therapy.”
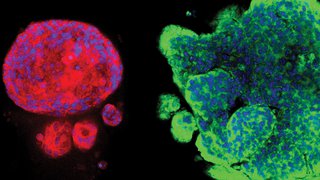
Dr. Alluri will lead translational studies aimed at understanding the determinants of response or resistance to radiation therapy in breast cancer patients. These studies will employ innovative technologies, such as spatial transcriptomic and proteomic profiling in tumor samples collected from patients participating in this trial.
“Traditionally, patients receive breast radiation to eliminate any residual microscopic disease after they have undergone surgery,” Dr. Alluri says. “This makes it challenging to assess how a certain patient has responded to their radiation treatment as the visible portion of the tumor has already been removed at the time of surgery.
“This novel clinical trial will offer an unprecedented opportunity to unravel the underlying biology that drives the variability in response between patients to breast radiation, thereby enabling us to develop future treatments that are personalized to the individual biology of each patient,” he adds.

Next Generation of Kidney Cancer Immunotherapies
The second clinical trial called SPARK will test a novel STING agonist, developed at UTSW, and personalized ultra-fractionated stereotactic adaptive radiotherapy (PULSAR®) in combination with immune checkpoint inhibition in patients with metastatic kidney cancer. It will be co-funded by the National Institutes of Health (NIH) Kidney Cancer SPORE, CPRIT, and ImmuneSensor Therapeutics. Raquibul Hannan, M.D., Ph.D., Professor of Radiation Oncology, Immunology, and Urology; Hans J. Hammers, M.D., Ph.D., Professor of Internal Medicine; and James Brugarolas, M.D., Ph.D., Director of the Kidney Cancer Program and Professor of Internal Medicine, are co-investigators on the trial.
This phase II clinical trial will evaluate combination IMSA101, SABR/PULSAR, and maintenance nivolumab in patients with metastatic clear cell renal cell carcinoma (ccRCC) who have been previously treated with immunotherapy.
“We’re setting the stage for the next generation of immunotherapies in RCC where simultaneous activation of the innate and adaptive immune systems unleashes the full anti-tumor potential of immunotherapy,” Dr. Hannan says.

Improving Response to Immunotherapy
According to Dr. Hannan, there is an unmet need in RCC to develop more effective strategies to amplify response to immunotherapy. He believes that the simultaneous activation of the innate and adaptive immune system together with immune system priming by stimulating antigen presentation with SABR/PULSAR could be an effective strategy.
“IMSA101 is a novel activator of the STING pathway,” Dr. Hannan says. “Our study is evaluating the impact of combining innate immune system activation, with the STING activator, that facilitates antigen release and adaptive immune system activation. This is the rationale for combining IMSA101 and PULSAR with maintenance nivolumab.”
In addition to assessing standard efficacy and safety endpoints, the team will perform single-cell RNA sequencing and immune profiling on tumor samples to determine the expression of STING target genes and several additional parameters that would provide insights into the mechanisms of induction of an anti-tumor immune response.
“This will be the first trial to combine a STING agonist with stereotactic radiation for patients with metastatic kidney cancer,” Dr. Hannan says.
Asal Rahimi, M.D., is Associate Professor of Radiation Oncology at UT Southwestern and a member of the Experimental Therapeutics Research Program at Simmons Cancer Center. She is Chief of the Breast Radiation Oncology Service, Medical Director of the Simmons Cancer Center Clinical Research Office, and Associate Vice Chair for Program Development in Radiation Oncology.
Basak Dogan, M.D., is Professor of Radiology in the Breast Imaging Division and Director of Breast Imaging Research at UT Southwestern. She is a Eugene P. Frenkel Endowed Scholar in Clinical Medicine. She is an affiliate member of the Cellular Networks in Cancer Research Program at Simmons Cancer Center.
Prasanna Alluri, M.D., Ph.D., is Assistant Professor of Radiation Oncology at UT Southwestern and a member of the Experimental Therapeutics Research Program at Simmons Cancer Center. He specializes in the treatment of breast cancer.
Raquibul Hannan, M.D., Ph.D., is Professor of Radiation Oncology, Urology, and Immunology at UT Southwestern, where he serves as Chief of the Genitourinary Radiation Oncology Service. He specializes in the treatment of genitourinary cancers, including kidney cancer, and is a member of the Experimental Therapeutics Research Program at Simmons Cancer Center.