Treatment for Familial Hypercholesterolemia
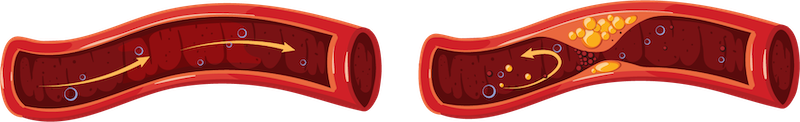
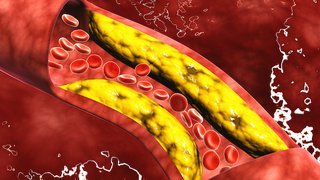
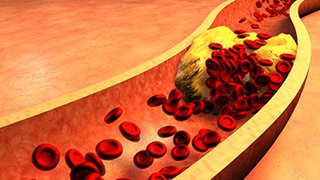
Proper treatment can successfully lower LDL cholesterol levels and reduce the risk of atherosclerosis, heart disease, and heart attacks. Our FH specialists work closely with patients to create treatment plans that are customized to each patient’s individual needs.
We treat FH with lifestyle changes and medications to control blood levels of LDL cholesterol and to lower risks of heart attacks and strokes. Our recommendations for healthy habits include:
- Heart healthy diet with less saturated fat, less cholesterol, and more fiber
- Physical activity
- Weight loss, for people who have excess body weight
All patients with FH will need medications to reduce LDL levels. Diet and exercise alone will not be enough to lower the LDL to good levels with this genetic condition. Options for medications include:
- Statins to reduce the liver’s production of cholesterol and help remove cholesterol from the blood
- Cholesterol absorption inhibitors that reduce the amount of dietary cholesterol absorbed by the small intestine into the bloodstream
- Bile-acid-sequestering resins that bind to bile acids, stimulating the liver to use excess cholesterol to produce more bile acids needed for digestion
- Injections of cholesterol-lowering medications referred to as PCSK9 inhibitors
For people who have extremely high blood levels of LDL cholesterol, UT Southwestern is one of the few centers in the country that offers LDL apheresis. In this procedure, small amounts of blood or plasma are removed from the body, processed through special filters to remove extra LDL cholesterol, and returned to the body.
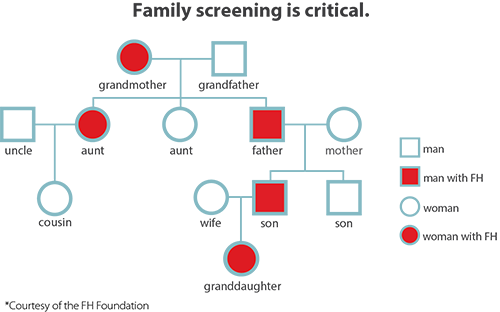
Family screening is critical since up to half of close family members, including children of patients with FH, will also have FH. Family screening includes:
- Checking cholesterol levels in close relatives
- Doing genetic testing in families to confirm diagnosis (cascade testing)
- Connecting to our pediatric partners specialists who treat FH when children are diagnosed
Support Services
UT Southwestern offers specialized services to support patients with heart disease and their families. Learn more about our heart support services.
Clinical Trials
Our FH specialists continue to be active in research to improve treatment. We are involved in an ongoing trial for homozygous FH. We are also a site for the national CASCADE FH registry, in which patients can get access to the latest care options and information.