8 essential health screenings for chronic and seasonal conditions
March 9, 2020

In some ways, being a doctor is like being a detective. We use our knowledge, instincts, training, and advanced technology to uncover clues and help our patients maintain good health.
Screening tests are some of the most valuable sleuthing tools we have at our disposal, particularly to dismiss or detect the presence of certain diseases, viruses, or chronic health problems. That’s one reason screenings for conditions such as high blood pressure or high cholesterol have become a standard part of routine physicals.
And at certain times of the year, we regularly screen for influenza or other infectious diseases, such as the novel coronavirus COVID-19. Those screenings are particularly vital because they can assist in the rapid identification of a patient who could transmit an infection to others.
SEE THE SCREENING PROTOCOL FOR INFECTIOUS DISEASES
While screenings don’t necessarily solve the case, they can guide us to the best diagnostic tests and techniques that will ultimately catch the culprit.
In a word, screenings can be lifesavers.
Here are some of the most common screenings we recommend for patients on a regular basis, and the screening protocol we use during flu season or during an outbreak of infectious disease:

The screening: Cholesterol
What it is: A blood test that can check for elevations in LDL (“bad” cholesterol) and triglycerides, and reductions in HDL (“good cholesterol), all of which can increase your risk of heart disease and stroke.
When to get it: The American Heart Association recommends getting cholesterol levels checked every five years beginning at age 20. Consult your physician, though, because screening age varies based on risk factors such as obesity, diabetes, and a family history of high cholesterol.
How it helps: Early detection can lead to preventive measures, such as lifestyle modifications or medications to keep your cholesterol under control.
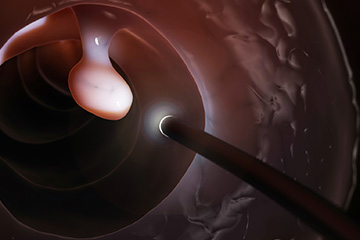
Colonoscopy
What it is: The most effective colon cancer screening technique, colonoscopy is a minimally invasive procedure that involves the insertion of a scope containing a tiny camera to view the entire colon. It can detect polyps before they become cancerous and also help find other diseases of the gastrointestinal tract, such Crohn’s disease and ulcerative colitis.
When to get it: For patients at average risk for developing colorectal cancer, colon cancer screening should begin at age 45. The frequency of repeat colonoscopies will be determined based on the findings of each patient’s results.
How it helps: One of the most significant advantages of a colonoscopy is the physician can remove precancerous polyps found during the procedure and have them biopsied. In many cases, colonoscopy can prevent the polyps from ever developing into cancer.

Depression
What it is: A team at UT Southwestern has developed an innovative screening method called VitalSign6. It uses a web-based application and allows primary care, pediatric, and specialty clinics to quickly screen for depression.
When to get it: During annual checkups or when you think you may be experiencing symptoms of depression.
How it helps: One in six adults in the U.S. will experience depression at some point in their lives. Regular screening can help detect the problem and provide treatment strategies.

Diabetes or prediabetes
What it is: A blood test to determine glucose levels and potential risk for Type 2 diabetes.
When to get it: The American Diabetes Association recommends screening for anyone over age 45, or for a person of any age if their body mass index (BMI) is greater than 25 and they have another risk factor, such as a family history of diabetes.
How it helps: A fasting glucose blood test result with a value of 126 mg/dL or higher is considered diabetic. A reading of 100 mg/dL indicates prediabetes. The blood glucose test can identify type 2 diabetes risk early and allow for medical and/or lifestyle therapies.

Mammography
What it is: Mammograms are the most powerful tool to detect breast cancer.
When to get it: Patients can schedule a mammogram without a referral from a physician if they are over age 40. The American Cancer Society recommends beginning annual mammograms at age 45. UT Southwestern’s Center for Breast Care at Harold C. Simmons Comprehensive Cancer Center recommends a clinical breast exam starting at age 20 along with an annual mammogram starting at age 50 for women at average risk for breast cancer. Women at higher risk should talk to their doctors about a more frequent screening schedule.
How it helps: X-rays are used to create an image of breast tissue, which can detect abnormalities such as tumors or cysts and lead to early treatment. Mammograms also provide peace of mind, knowing your breast tissue is clear.

Obesity
What it is: The Centers for Disease Control and Prevention (CDC) defines obesity as a BMI of 30 or higher. BMI, or body mass index, is a measurement that divides a person’s weight by the square of their height.
When to get it: Annually, at least. BMI is easy to check with an online calculator such as the one offered by the CDC, which will also provide normal and overweight ranges for your height.
How it helps: Approximately 38% of Americans are obese, which many experts consider epidemic levels. If you can avoid obesity, you reduce your risk of cardiovascular diseases, diabetes, stroke, cancer, and other potentially life-threatening illnesses.

Pap smear
What it is: A Pap smear involves collecting cells from the cervix to screen for cancer.
When to get it: The U.S. Preventive Services Task Force (USPSTF) recommends a Pap smear every three years for women 21 to 65, for women 30 to 65, and HPV testing every five years. All preteens should get the HPV (Human Papillomavirus) vaccine at age 11 or 12, according to CDC recommendations. If the preteen immunization was missed, women can still get the HPV vaccine up to age 26. Men are eligible for the vaccine up to age 21. Recent guideline changes have extended the age for the HPV vaccine to 45 in certain instances.
How it helps: Almost all cases of cervical cancer are caused by HPV, a sexually transmitted cancer that can be prevented by vaccine. Early screening can help prevent HPV from leading to cervical cancer.
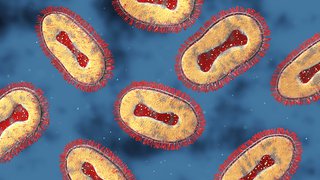
Viral respiratory infections

What it is: UT Southwestern’s infectious disease specialists have developed a screening protocol that involves immediately identifying those who have potential respiratory or other infectious diseases and providing masks and isolation for further screening. Our intake coordinators are trained to ask an initial round of questions about recent travel to areas where infections have been common, people you may have associated with who may have infections, and the time frames of when symptoms developed.
When to get it: During the influenza and respiratory virus season, which extends from September to May, medical facilities such as UT Southwestern routinely screen all patients (and sometimes visitors) for fever or other symptoms such as cough, shortness of breath, runny nose, sore throat, etc. If any of these are positive, the patient (or visitor) is given a mask and might be taken to a private room or separate waiting area away from individuals who may not be ill.
How it helps: In the time of emerging infections – such as COVID-19 – the screening tools assist in the rapid identification of patients who could be infected and at risk of transmitting infection to others. The final decision whether to test an individual takes into account the responses to the screening tools and is ultimately determined by the local health department in discussion with the CDC. Blood and respiratory samples may be taken for testing of a variety of conditions including flu or COVID-19 at UT Southwestern labs.
For more on COVID-19 screening, preparedness, and response at UT Southwestern, please go to our COVID-19 website.