One complex lung surgery makes a lifetime of difference
October 30, 2025
By Renee Yan
Two years ago, Dan Dudley could not cross a room or even get out of bed without feeling faint, lightheaded, and out of breath. Taking 12 steps felt like running 500 miles, he said.
Dan didn’t know it at the time, but he was exhibiting classic symptoms of chronic thromboembolic pulmonary hypertension (CTEPH), a rare disease where blood clots scar into the arteries of the lungs and impair blood flow. Ultimately, CTEPH forces the heart to squeeze harder to pump blood throughout the body, and can be potentially deadly, so Dan would need a complex, 10-hour surgery known as a pulmonary thromboendarterectomy (PTE) to save his life.
Living in Amarillo, Dan’s options for such a specialized procedure were limited. His pulmonologist directed him to UT Southwestern, about 360 miles away, where the team at the accredited Pulmonary Hypertension Center of Comprehensive Care is well-equipped to diagnose, assess, and treat CTEPH. UTSW has been establishing itself as a leading PTE center over the past eight years.
The referral, Dan believes, changed his life.
“The care I got, not just from the doctors but from staff at the entire hospital – it’s given my life back to me,” he said. “That’s a real special thing.”

Sonja Bartolome, M.D., Medical Director of the Pulmonary Vascular Disease Program, said her team is accustomed to treating CTEPH patients who travel from surrounding Texas cities and nearby states.
“We started our chronic thromboembolic pulmonary hypertension program in 2017, and we did so because there were many patients in our region who were not able to get the specialized care that they needed,” Dr. Bartolome said. “Our vision for the PTE program is really one of service.”
Dan’s case was further complicated as, eight years ago, he had previously undergone a quadruple cardiac bypass surgery that used four grafted blood vessels to create new pathways for blood flow around his heart. This meant Dan needed a re-operative procedure, and the scar tissue from that past surgery presented an added layer of risk.

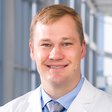
Christopher Heid, M.D., Assistant Professor of Cardiovascular and Thoracic Surgery, had to avoid disturbing these vital bypass grafts while still removing all the clots and scar tissue, which were obstructing much of the blood flow in his left lung and nearly completely in his right lung. To say it was a challenge is an understatement.
“This operation is one of the more complex ones that UT Southwestern, or any other institution, does,” said Dr. Heid, who expressed confidence because he knew he was backed by a multidisciplinary team of radiologists, care coordinators, pulmonologists, cardiologists, anesthesiologists, nurses, and intensive care specialists who would help him support Dan’s care and recovery.
“CTEPH patients require meticulous care,” he said. “And our pulmonary hypertension program is uniquely qualified to offer that kind of comprehensive care all in one location.”
What causes CTEPH?
Dan said his health had been on the decline for several years, but he initially attributed that to old age. He is 78 now.
He endured three bouts of pneumonia due to sinus drainage that caused fluid to build up in his lungs. Dan’s respiratory issues worsened following a bout with COVID-19.
That’s when the pulmonologist in Amarillo discovered a blood clot in his lungs, and despite taking blood thinners, Dan’s condition worsened. He required more advanced care.
This is not an uncommon scenario for CTEPH patients, Dr. Bartolome explained. In the United States, pulmonary embolism and deep vein thrombosis affect about 900,000 people every year, according to the American Lung Association. Most are able to return to their normal lives without issue after taking blood thinners, but in approximately 2% of cases, clots will linger and get worse, scarring and obstructing the pulmonary blood vessels, according to a study in the Journal of the American Heart Association.
As these scarred-in blood clots obstruct and narrow the lung blood vessels, the right side of the heart has to squeeze harder to get the blood through – similar to when a pipe in your home plumbing gets plugged up. Over time, the added stress on the cardiac muscle leads to right-sided heart failure. The severity of CTEPH is measured by how much trouble the right side of the heart has when pumping blood through the lungs, Dr. Bartolome said.
People with blood clotting disorders or health conditions that promote clotting have a greater risk of developing CTEPH. This includes patients diagnosed with cancer or chronic inflammatory disorders, patients who have undergone a surgery to remove their spleen, or those who have longstanding intravenous lines or other implanted devices.
COVID-19 infections are also linked with a higher rate of pulmonary embolism, but the majority of the time, patients develop CTEPH without any known risk factors, Dr. Bartolome added.

This was the case for Dan, whose condition continued to deteriorate.
“Mr. Dudley came in with persistent shortness of breath with exertion,” she recalled. “When I met him, he really couldn't walk very far, so it was affecting his quality of life. He was starting to have swelling in his feet, and that happens from failure of the right side of the heart.”
Dr. Bartolome and her team performed a series of assessments to confirm the diagnosis and determine whether Dan would be a suitable candidate for surgery. This included computed tomography angiography (CTA), echocardiography, ventilation/perfusion scanning, a right heart cardiac catheterization with pulmonary angiography, and multiple lung and heart function tests. Using these tests, doctors are looking for red flags, such as enlarged heart chambers, backflow of blood, and pressure in the pulmonary blood vessels.
Dan’s lung images showed large scarred-in blood clots, and his echocardiogram indicated the blood pressure in his lungs was double what it should be. As a result, he had poor function on the right side of his heart, and the distance he could walk comfortably was cut in half.
“Surgery was our first and best option in this case,” Dr. Bartolome said. “In a given year, we are referred between 100 and maybe 150 cases. Amongst those cases, not everybody will be a surgical candidate, and we have other things that we can do. But for patients like Dan, surgery is the best and most proven treatment in getting patients back to a normal lifespan and a normal quality of life.”
Related reading: Warning signs when an artery is blocked, and how to fix it
A surgical solution that provided ‘instant relief’

In January 2025, Dan checked into UT Southwestern's William P. Clements Jr. University Hospital, where Dr. Heid and his team prepped him for a pulmonary thromboendarterectomy (PTE).
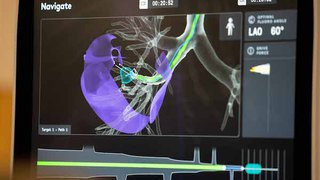
During this highly specialized procedure, patients are sedated and connected to a bypass machine, which temporarily takes over the functions of their heart and lungs. Their body temperature is gradually lowered to around 65-68 degrees Fahrenheit to a state of deep hypothermic circulatory arrest, which slows the body’s metabolism and diminishes the need for oxygen. This allows surgeons to halt the flow of blood for short periods so they can access the intricate network of peripheral pulmonary arteries connecting the heart and lungs and tease out the life-threatening scarred-in clots.
“By removing the clots and scar tissue lining the blood vessels, we effectively reduce their pulmonary hypertension and the stress on the heart’s right ventricle, thereby alleviating the patient’s heart failure,” Dr. Heid said. “Time is truly of the essence because we are using periods of deep hypothermic circulatory arrest. We have to limit the period of circulatory arrest to 20 minutes at a time, separated by 10 minutes of reperfusion.”
For 10 hours, Dr. Heid and a care team of more than a dozen worked in the operating room. Dan had severely elevated pulmonary vascular resistance.
Despite the complexity of the procedure, Dr. Heid successfully removed these blockages. By placing Dan in a deep hypothermic circulatory arrest, the surgical team created a bloodless field that allowed Dr. Heid to make incisions in the main pulmonary artery on each side. Through the small openings, he was able to visualize and access the peripheral branches. He used specialized instruments to carefully remove all the clots, and upon finishing, he even corrected a sternal alignment issue that never healed properly after Dan’s previous bypass procedure.
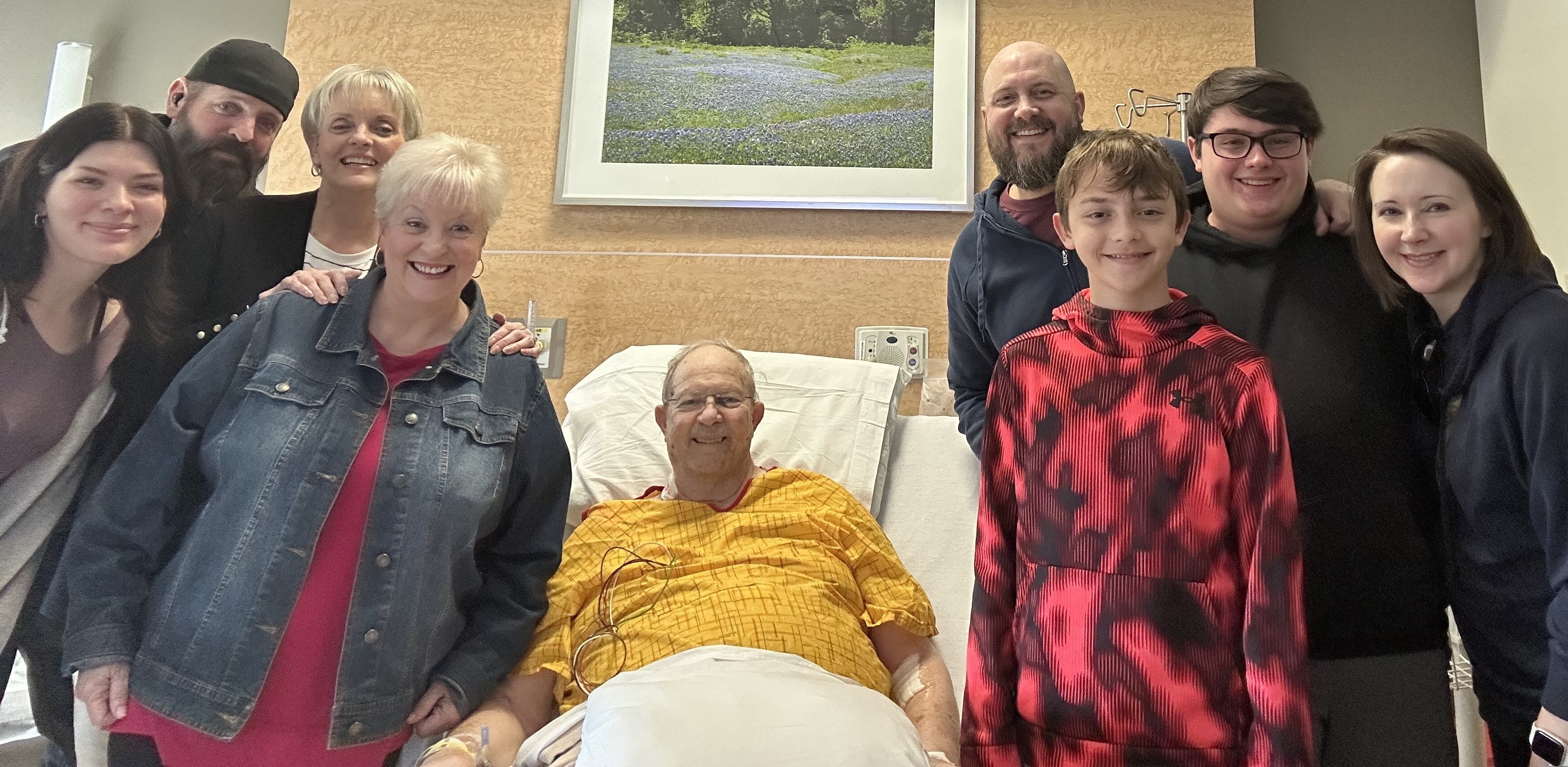
Afterward, Dan noticed an almost immediate improvement.
“It was an instant relief of being able to breathe. It made me feel like I was 10 years younger,” Dan said. “And because Dr. Heid fixed up my sternum, I found that it didn’t hurt anymore when I needed to cough!”

While most patients take several days, sometimes even weeks, to recuperate, Dan said he felt ready to go home by day two. The change in his condition was dramatic.
“Mr. Dudley’s breathing tube came out almost right away. He had no early post-operative complications and excelled,” Dr. Heid said. “To see people who come to the hospital who are short of breath, on oxygen, and barely able to walk – to see and help them essentially return to normal life is one of the most gratifying aspects of the job.”
Since January, Dan has continued to come to UTSW from Amarillo for follow-up appointments.
“He's doing really well post-surgery,” Dr. Bartolome said. “He’s getting back to a great quality of life with his family.”
After a period of physical rehabilitation, Dan is now able to do what means the most to him: spending time with his family and sharing some of his favorite hobbies with his five grandchildren.
“We fish, we hunt, and we play golf,” Dan said. “I couldn't do that before this surgery because I couldn't walk that far. Now, I get to watch the kids learn all these new things.”
He credits his care team at UT Southwestern for giving him that gift.
“I’ve said it before, and I’ll say it again,” he said. “From the bottom of my heart, thank you.”
To talk with an expert about pulmonary thromboendarterectomy (PTE), make an appointment by calling 214-645-6616 or request an appointment online.