In a pandemic, even when you do everything right, viruses can still find a way into your home.
As a respiratory specialist, I have lived in PPE for the better part of a year and made sure that my family has taken every precaution. I was also among the first health care workers to be vaccinated. So when my husband, Ivan, got COVID-19 this winter, it was a stark reminder of just how insidious and unpredictable the SARS-CoV-2 virus can be.
Ivan didn’t have a mild case, either. He was sick with a fever and cough for two weeks straight. When I posted an update about Ivan's condition to my social media, I was surprised how many people came out of the woodwork and said, "I had it, too!" or "My whole family caught it at the same time!"
It was as if they felt ashamed of being infected by a novel coronavirus that has spread to nearly 29 million people in the U.S. They also seemed worried about being judged by others: What were you out doing? Didn't you wear a mask or wash your hands?
Leading up to Ivan's illness, we hadn't really gone anywhere or done anything. We never went out in public without masks on and hand sanitizer in tow. But that's what viruses do. They are always searching for an available host, even when we do our best to be careful.
As we approach the one-year mark of living with COVID-19, we need to eliminate the stigma and shift our focus to controlling the controllables, particularly as new variants to the SARS-CoV-2 virus arise. The vaccines, while vital, don’t mean we can let our guard down.
If someone in your immediate family becomes infected, there are steps you can take to reduce the risk and limit the spread at home. We developed an action plan when Ivan tested positive for COVID-19, and I wanted to share our experience in hopes it might help others.

1. Get tested early
When Ivan first started feeling sick, we thought it might be a cold or flu and not COVID-19. But just to be sure, we all got tested right away. My tests came back negative, and we were surprised when his were positive. More severe symptoms began shortly thereafter.
My children and I got tested a second time just to be sure, and we were still negative. Testing helped us isolate him early, potentially sparing the rest of the family from infection. Explore UT Southwestern testing options.

2. Isolate at the first sign of symptoms
Even before his test results came back, Ivan self-isolated at the first sign of symptoms. We're fortunate to have a bathroom off the master bedroom, which he was able to use through his two-week isolation. I took the spare room, main bathroom, and kitchen so I could bring him food throughout our time apart. I also worked from home, attending meetings and seeing patients via video conferences.
Ivan and I set up a protocol. I’d mask up, then knock. He’d put on his mask and move at least six feet from the door. I'd place his food on a side table, chat a bit, then leave so he could unmask and eat. When he was through, we'd repeat the process to clear away the dishes.
Our master bedroom has an external door, so we could see him through the glass if we stood in the yard. We could FaceTime, but it was difficult being apart for that long. I empathize with people who have had to deal with this situation throughout the pandemic with relatives in nursing homes and hospitals.
3. Divide and conquer
Not everybody has access to separate bedrooms and bathrooms. In tight quarters, do your best to keep people who have COVID-19 or symptoms in one area of the home and those who are well in another.
We know families who live in their RVs. When one person got infected, that person stayed in a room at the back of the RV, leaving only to use the restroom (masked up, of course). The rest of the family stayed out of the person's space, masked up, and used antiviral cleaners to wipe down the doorknobs, toilet handle, and faucets. No one else in the family got sick.
Do your best in your environment. Keep at least six feet of distance between sick and well individuals for at least 14 days after a positive COVID-19 test and after they've been fever-free for 24 hours. Keeping them isolated behind a door is safest, but physical distance may suffice. Weather permitting, spend time outdoors at home as much as possible. The virus is more likely to spread in closed in spaces without much ventilation.
Related reading: Tired of social distancing? Try NPIs on for size
4. Wear PPE at home when someone is sick
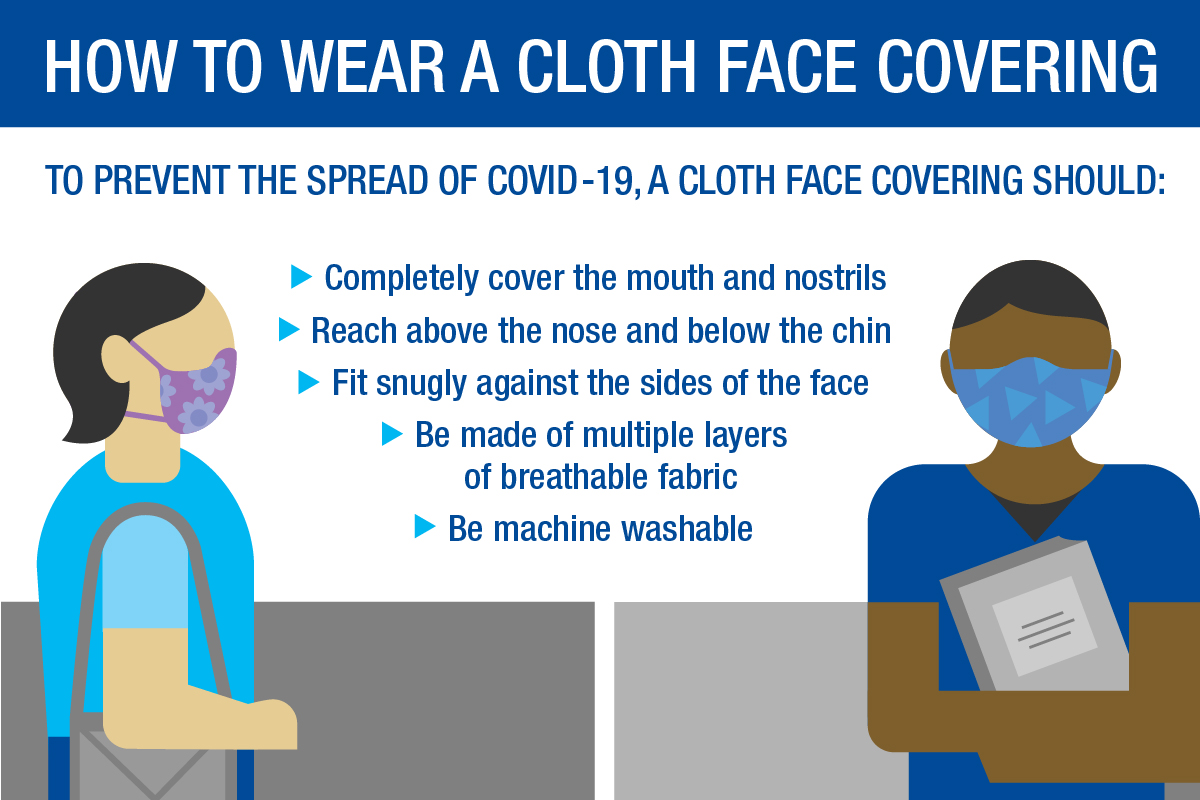
Most of us don't love wearing masks, but they make a difference. At work, I wear an N95 mask, face shield, gloves, gown, you name it. But at home, we wore simple surgical masks, and the virus did not spread to anyone else in our home.
Some of the recently recorded COVID-19 variants appear to spread faster than the original SARS-CoV-2 virus, but they do not appear to cause more severe infections. The Centers for Disease Control and Prevention (CDC) recently reiterated the importance of wearing a snug-fitting mask and even suggested wearing two masks, depending on the type, to further reduce the risk of exhaling or inhaling respiratory droplets.
5. Consider new treatments to avoid hospitalization
If you test positive for COVID-19 and are at high-risk for severe symptoms, consider getting a monoclonal antibody infusion. This new treatment consists of laboratory-made proteins that mimic how the immune system fights viruses. While the infusion doesn't cure COVID-19 infection, it can help decrease the viral load by blocking the virus from entering more cells. The goal is to reduce the severity of infection and avoid an ER visit or hospitalization.
Patients 12 and older who are hospitalized with COVID-19 may benefit from remdesivir, an antiviral medication that interrupts virus production, lowering its ability to multiply.
Research suggests that fewer than 3 percent of patients have mild side effects from the infusion. Perhaps the main drawback on monoclonal antibody treatment is that you can’t get a COVID-19 vaccine for 90 days afterward because the treatment may impair your body's immune response to the vaccine. However, it is rare to get infected with COVID-19 again in that timeframe due to the nature of the virus.
Texas has set up monoclonal antibody infusion centers around the state, including at UT Southwestern. Your primary care provider must refer you for treatment, which is under an emergency use authorization because it is so new. Find a center near you.
Related reading: Hair dryers and hydroxychloroquine - separating COVID-19 myths from realities
Building Confidence in the COVID-19 Vaccines
Vaccine hesitancy runs deep in the U.S., particularly in hard-hit communities of color. Dr. Quinn Capers, Associate Dean for Faculty Diversity at UT Southwestern and a national leader on the issue of diversity and inclusion in medicine, says the key to connecting with Black and Hispanic patients is delivering on a message of trust and equality.
6. Get vaccinated – even if you've already had COVID-19
The vaccine supply is limited right now, but that won't always be the case. As soon as you are eligible, you can schedule a vaccination appointment at UT Southwestern's Vaccination Page.
Around the time my husband recovered from COVID-19, he became eligible for the vaccine because he has a high-risk condition. He registered right away, but he did get some questions from friends who thought once you had the virus you were immune. That’s a common misconception. Nobody is sure how long natural immunities last, and while reinfections aren't common there are enough recorded cases that the CDC has recommended vaccination for people who have been infected with the virus.
It may sound cliché, but none of us are safe until all of us are safe. That’s why it’s important to get vaccinated when your time and opportunity come.
The potential side effects from a COVID-19 vaccine are minor and short-lived, especially when compared with the symptoms of COVID-19 infection for a patient who has comorbidities such as blood pressure, diabetes, or obesity. If you feel hesitant about getting vaccinated, talk with your primary care provider about your personal risk/benefit balance.
A few closing thoughts
Patients sometimes ask, "Why me? Why did I get this when I am so careful?" The truth is, viruses don’t discriminate – they just look for any way to spread.

That’s why it's essential to continue following COVID-19 safety protocols:
- Wear a mask
- Wash your hands
- Practice social distancing
- Avoid large indoor gatherings
- Get tested early and often
- Self-isolate if you feel sick or suspect you've been exposed
There shouldn’t be a stigma attached to catching COVID-19. Do your best to implement the precautions, and if someone in your family gets infected, do everything you can to limit the spread to the rest of your family and the community. Working together, we can beat this virus.
To visit with a primary care or respiratory health doctor, call 214-645-8300 or request an appointment online.