Life cycle of a coronavirus: How respiratory illnesses harm the body
April 2, 2020

Respiratory infections are among the most common diseases that affect humans. These illnesses can range from mild colds to serious lower respiratory tract infections such as bronchitis and pneumonia.
Many respiratory infections are caused by coronaviruses, a family of viruses that are easily spread through respiratory droplets in the air and on surfaces. The novel strain COVID-19 is the cause of the current worldwide pandemic.
In some patients, moderate upper respiratory infections can progress into serious lower respiratory infections within a few weeks. Patients whose symptoms began with a mild cough may develop respiratory failure, needing ventilator support to breathe.
How can a microscopic virus wreak such havoc in the body so quickly? And why do some patients (including men) get hit harder with respiratory illnesses?
Let’s take a closer look at what happens when a respiratory virus, such as COVID-19, enters the body, as well as how we can protect ourselves and others.
COVID-19 can move from the upper to lower respiratory tract
Viral respiratory illnesses typically spread when an infected person coughs or sneezes, spraying germs into the air that land on surfaces. If you breathe in the respiratory droplets, or touch surfaces and then touch your face, the virus can enter your body and infect you.
COVID-19 is particularly contagious; one infected person, on average, spreads it to 2.2 people. By comparison, people with the seasonal flu typically spread it to about 1.3 people. The novel coronavirus also seems to infect the upper and lower respiratory tracts at a higher rate than other viruses, which creates more coughing and more potential for community spread.
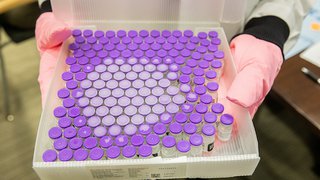
The Making of a COVID-19 Vaccine
See how the complex process works and how it has been accelerated to combat the pandemic. (Published in Oct. 2020)
Upper respiratory infections
The lungs are among the few organs besides the skin that are in constant contact with the outside world. This, along with ease of transmission through touch, increases humans' susceptibility to developing respiratory illnesses.
Once inside the body, viruses first enter the upper respiratory tract, which includes the nasal passages, throat (pharynx and larynx), and windpipe (trachea). The virus begins to replicate, invading your healthy cells.
- Symptoms: Sore throat, dry cough, shortness of breath, fever, headache, and fatigue.
- Treatment: Options generally include symptom management because antibiotics don't work against viruses. The doctor might suggest drinking plenty of fluids, resting, and taking over-the-counter medication to lower fevers and manage body aches, as well as decongestants for sinus trouble.
- Duration: Patients with upper respiratory infections typically feel sick for a week or two.
In most patients, the body’s immune system kicks in to fight the virus and contain it in the upper respiratory tract. It creates antibodies, which bind to the virus so it can't replicate, as well as T-cells, which attempt to destroy the virus. About 80% of people who are infected with COVID-19 have mild to moderate symptoms and recover without needing hospitalization or treatment by a specialist, according to the World Health Organization.
But if a patient has a weak immune system, or an especially aggressive infection, the virus can invade the lower respiratory tract and affect the lungs. These infections are typically more serious because they interfere with our ability to breathe.

Lower respiratory infection
If the virus progresses beyond the upper respiratory tract, it can begin to cause inflammation on our bronchial trees – the passages that conduct air between the lungs and the outside world.
In these cases, the virus targets the lung cells that make mucus, as well as those that have tiny hairs called cilia. Mucus protects lung tissue and keeps the lungs from drying out, while the cilia move the mucus and clear out debris such as pollen or viruses. Inflammation irritates the nerves in the lining of the bronchial trees, increasing sensitivity to even a tiny speck of dust.
To fight the virus, the immune system may go into overdrive, setting off an inflammatory response that fills up the air sacs in the lungs. Unfortunately, this response can render the cells unable to clear out debris and fluid. When the patient's airways become inflamed, pneumonia can set in.
- Symptoms: Severe cough that produces mucus, shortness of breath, tightness in the chest, and wheezing upon exhalation. In severe cases, the lips may appear blue due to low oxygen levels.
- Treatment: Options may include breathing treatments such as an inhaler, nebulizer or medication, as well as antibiotics if bacteria and a virus are involved. A humidifier or hot shower may ease chest discomfort and help you breathe.
- Duration: Mild to moderate lower respiratory infections typically resolve within two weeks.
If too much of the lung is damaged, the rest of the body doesn’t get enough oxygen, which can lead to organ failure. In these severe cases, a patient may need ventilator support to breathe.
What is a ventilator?
A ventilator is a piece of medical equipment that helps patients breathe via a tube placed down their throat and into the lungs (intubation). Using a ventilator will not cure the infection, but it can give the body time to heal and recover.
Most patients with respiratory infections will not need ventilator support. Still, it is important to understand how seriously illnesses such as COVID-19 can affect the body. And knowing the facts can serve as a reminder of why we must take preventive measures like handwashing and self-quarantines seriously.
Who is most at risk for respiratory illnesses?
Nearly all of us will contract a respiratory illness at some point during our lifetime. Anyone can become seriously ill from these infections, but some are at higher risk.
Research suggests that men develop more respiratory infections, typically with worse outcomes, than women. Data are similar for COVID-19, according to the provider-led publication Advisory Board, which states that women typically mount higher immune responses to viruses and present sooner for medical care than men.
Individuals most at risk for developing respiratory infections include those who:
- Are older than 65
- Live in a nursing home or long-term care facility
- Have chronic lung disease or asthma
- Have serious heart conditions
- Are immunocompromised, including those with cancer, immune deficiencies, prolonged corticosteroid use, or other immune-weakening medications
- Have underlying medical conditions, such as diabetes, kidney disease, or liver disease
COVID-19 has not shown an increased risk to pregnant women. However, pregnant patients should be monitored closely.
Related reading: COVID-19 and pregnancy: Answers to 10 key questions
When should you seek medical help for a respiratory infection?
If you have been exposed to a respiratory illness such as COVID-19 and develop a fever, cough, sore throat, or body aches, stay home and avoid other people. If you must be in close contact, wear a facemask and gloves to avoid contaminating others.
Avoid going to your doctor's office or urgent care unless your symptoms get worse, such as becoming short of breath doing normal activities, feeling like you’re breathing through a wet sponge, or wheezing.
Call ahead if you are experiencing mild to moderate symptoms. This will give us time to help protect other patients from infection. If it’s an emergency, call 911 and tell the dispatcher you suspect you may have COVID-19.
If you test positive for COVID-19, the recommended treatment will not necessarily change. There is no known cure for this (or any) coronavirus. But there are a few treatment options beyond rest and over-the-counter medications for more moderate to severe symptoms. Those include breathing treatments such as an inhaler, nebulizer, or antibiotics if bacteria and a virus are involved. A ventilator is only used in the most severe cases.
Related reading: Managing your mental health during a pandemic
How can people help reduce the spread of respiratory illnesses?
The latest data from the Centers for Disease Control and Prevention suggest that more than half of the U.S. is experiencing some community spread of COVID-19. While we can’t avoid every circulating illness, we can take precautions to reduce the spread of respiratory viruses.
The top preventive measure is to wash your hands frequently, following these five steps, every time:

If soap and water are not available, use an alcohol-based hand sanitizer with at least 60% alcohol.
Additionally, all of us must take physical isolation guidelines seriously. If possible, work from home. Avoid going out unless it's absolutely necessary. And make sure your family members are doing the same.
People can carry the virus to others without ever developing symptoms. We also know the virus can live for hours in the air and several days on surfaces – it is up to all of us to stay home as much as possible to help stop the spread and contain COVID-19.
I know this can be a stressful time. If you have questions or concerns, we are here for you. Visit our COVID-19 information hub for the latest updates.