For millions of Americans, hearing loss affects communication, confidence, safety, and quality of life. It’s estimated that 1.2 million U.S. adults could benefit from a cochlear implant, but fewer than 10% get one.
Why the gap? Many people don’t know cochlear implants are an option for them. In fact, a 2022 survey found that 31% of people with hearing difficulty said they had never heard of a cochlear implant.
Some eligible patients worry that the sound from a cochlear implant will be robotic or that the device will be too visible – part of the device is worn on the scalp, behind the ear. Others may hesitate because the idea of having surgery can feel intimidating.
Cochlear implant technology has advanced significantly in the past decade. Getting these devices helps thousands of adults with hearing loss each year maintain independence, communication, and engagement with the world around them.
If you have questions about the devices or surgery, you’re not alone. Here are answers to 10 common questions about cochlear implants that we often answer for patients.
1. Am I eligible for a cochlear implant?
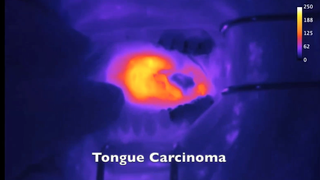
Cochlear implants bypass the damaged parts of the ear to directly stimulate the auditory nerve, which connects to the area of the brain responsible for processing sound.
Your eligibility to get a cochlear implant will be determined through detailed hearing tests performed by a cochlear implant-trained audiologist. Some of the criteria include:
- Having moderate to profound sensorineural hearing loss – the cause stems from damage to the inner ear, or cochlea, in one or both ears
- Having one or both auditory nerves intact
- Getting little or no benefit from hearing aids
- Being healthy enough to have surgery
Cochlear implants are most common in two groups of patients: infants born with profound hearing loss and adults over 65 whose hearing has declined over time from aging, genetics, or noise exposure.
However, people of any age with hearing loss caused by trauma, an infection, certain medications, or autoimmune disease may benefit from getting a cochlear implant.
Young children tend to receive cochlear implants in both ears, while older adults may get an implant in only one ear. Some patients have a cochlear implant in one ear and use a hearing aid in the other. Each case is different.
Specialists in the UT Southwestern Department of Otolaryngology can evaluate any patient who is interested and help determine whether cochlear implants could restore or improve their hearing.
2. Am I too old to get cochlear implants?
Age alone is never the limiting factor. What matters is overall health (including cognitive health), the type of hearing loss, and motivation. We routinely place implants for patients in their 70s, 80s, and 90s, and many report significant improvements in their quality of life.
There is growing evidence that people who lose their hearing during midlife are at increased risk of developing dementia. The link between hearing loss and dementia is not fully understood, though it likely involves the isolation that occurs when people withdraw from social situations due to their hearing problems.
Social isolation and depression are both risk factors for dementia. Treating hearing loss can help lessen social isolation and may play a role in reducing cognitive decline.
3. How bad does my hearing have to be before I consider cochlear implants?
It’s a common misperception that you must be completely deaf to benefit from cochlear implants. In reality, it’s better not to wait. The longer the brain goes without meaningful sound, the harder it becomes to adapt to a cochlear implant. For adults, a decade or so of severe hearing loss may negatively impact the outcome.
If hearing aids no longer help you hear clearly, especially when it comes to understanding speech, it may be time to consider an implant. Earlier implantation often leads to better speech understanding and overall satisfaction.
4. Will I lose all my natural hearing?

Many people worry about this, and it’s an important conversation to have with your audiologist and surgeon. It used to be that inserting the implant would almost certainly result in the loss of remaining natural hearing in the ear.
Now, we can often preserve some residual hearing due to advances in electrode designs and surgical techniques, such as:
- Smaller, thinner electrodes
- Slower, gentler insertion techniques
- Steroids prescribed to patients before and during surgery to protect the inner ear
We still counsel patients to expect the loss of some or even all of their natural hearing in the implanted ear. However, the improvement from the implant usually far outweighs what the ear could provide naturally.
It is important to note that after you get a cochlear implant, you may not be able to go back to using a hearing aid in that ear. Cochlear implants are designed to bypass the damaged portion of the ear, and in some cases, that part may not work after the surgery. In some cases, an aim for hearing preservation may be undertaken for patients who have good low frequency hearing but are profoundly deaf in the higher frequencies.
5. How long will it take after surgery to hear again?
Cochlear implants traditionally were activated two to three weeks after surgery. UT Southwestern has adopted early activation, sometimes next day. This is a new approach that early research shows may help patients adapt to the implant faster.
After your cochlear implant is activated, your hearing won’t be at peak quality right away. It takes time to retrain the brain to understand the sounds it receives from the device. Consistent, everyday use of the implant after activation will also help your brain adapt.
After working with your audiologist to fine-tune the implant and practice using it, you’ll usually start experiencing significant benefits within three to six months. After a year most patients are doing very well with their cochlear implants. Getting used to the devices takes patience, but nearly everyone we treat says it’s worth it.
6. What will music sound like with a cochlear implant?
This is a great question, and it’s important to set realistic expectations. A cochlear implant stimulates groups of frequencies rather than individual hair cells, so the sound is different from natural hearing.
At first, sounds may seem electronic, robotic, or like white noise. That’s normal, and the brain is remarkably adaptable. You won’t hear as well as you might have in your teens. But over time, voices and other sounds should become clearer, more natural, and easier to distinguish.
Music can be more challenging because the implant has a limited frequency resolution. You’ll likely still enjoy your favorite songs because your brain remembers them, but it can be challenging to learn new music. Patients who have a cochlear implant in one ear and hearing in the other ear (with or without a hearing aid) often get enjoyment from music using both technologies together.
7. How long do cochlear implants last?
The internal implant is designed to last a lifetime. Unlike battery-powered medical technologies such as pacemakers, the power source for a cochlear implant is external. Nothing needs to be replaced unless the device is damaged or stops working, which is rare.
The external processor can be upgraded as technology improves, and the implant itself stays in place. In fact, patients who got some of the first cochlear implants in the 1970s still use their original devices today!
8. What is the process to get a cochlear implant?
While the surgery is quick, the evaluation process is comprehensive. Our goal is to ensure you are a good candidate and will benefit from the technology before we recommend surgery.
The evaluation and implant process typically involves these steps:
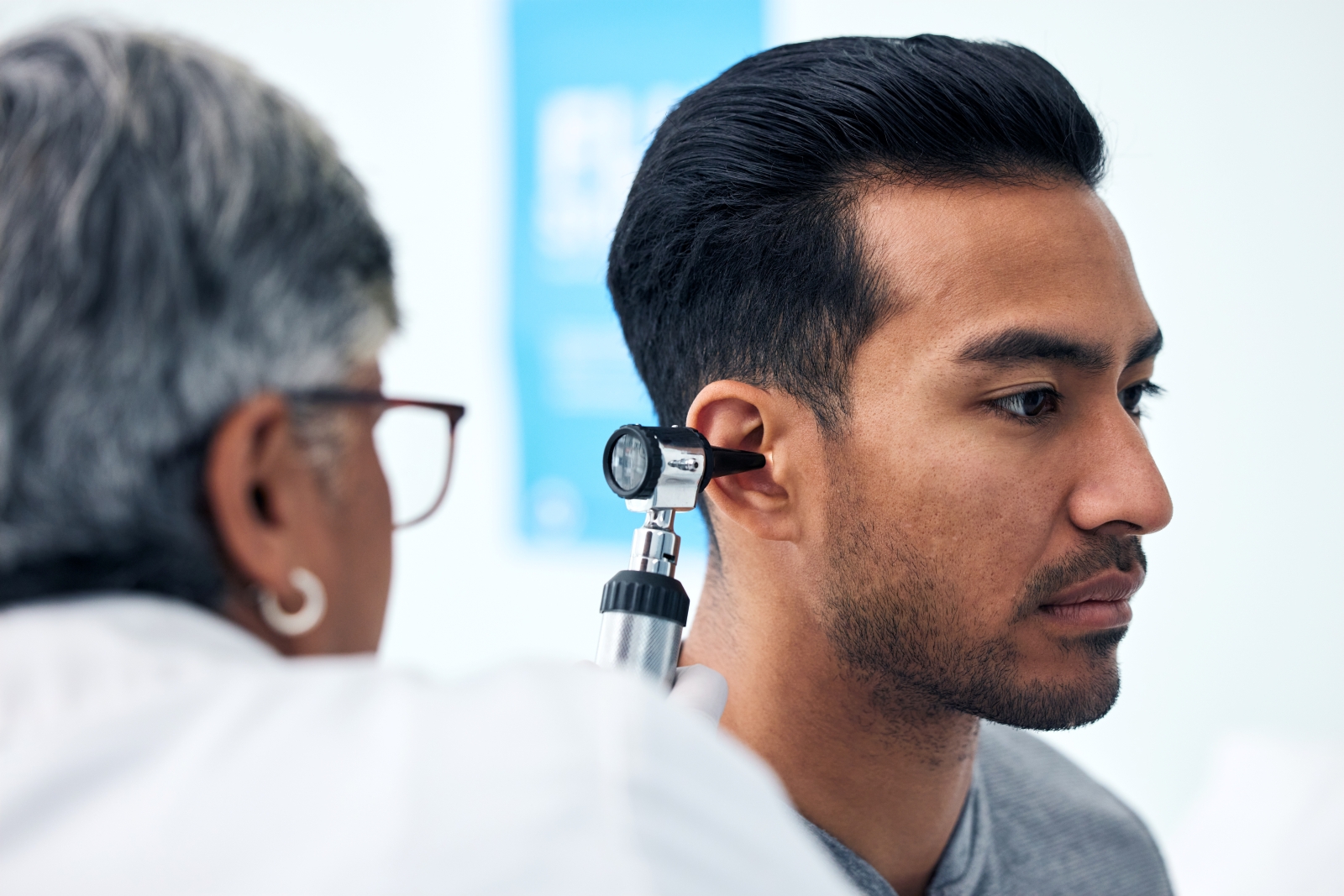
- Referral from an audiologist or ear, nose, and throat doctor (otolaryngologist)
- Detailed hearing tests with a cochlear implant audiologist
- A meeting with the surgeon and audiologist to review risks, expectations, and device options
- Surgery, which is usually a one- to two-hour outpatient procedure
- Activation shortly after surgery
- Regular mapping and rehabilitation to adjust the device and help retrain your brain to interpret sound in a new way
9. What should I expect during cochlear implant surgery?
Cochlear implant surgery is generally a safe, well-tolerated outpatient procedure that takes one to two hours.
You will be asleep under general anesthesia, and a small incision will be made just behind the ear. We will remove the mastoid bone, which is a small bone under the ear. This allows us to access the middle ear without having to pierce the eardrum.
We implant the device through a structure called the round window – a flexible membrane in the middle ear that releases pressure and helps transmit sound energy to the fluid in the cochlea. This newer technique has decreased inner ear trauma and improved hearing preservation rates.
Next, we place the external receiver/power source behind the ear, under the skin. It will be secured in place, and we will test it to ensure the device is aligned and functioning properly. Then the surgeon closes the incision and covers the wound with a dressing before you head to the recovery room to wake up from anesthesia.
You can go home the same day, and most patients resume normal activities within a few days. We can send you home with pain medication, but many patients find over-the-counter acetaminophen or ibuprofen controls any discomfort. You also may have temporary dizziness in the first couple days after surgery.
Self-coiling cochlear implant could transform care for severe to profound hearing loss
- Kenneth Lee, M.D., Ph.D.
August 24, 2022
10. Who should I trust to do my surgery?
As with any surgery, experience matters in surgical technique and in guiding you through life with a cochlear implant. UT Southwestern specialists perform more than 150 implants here and through the UT Pediatric Cochlear Implant Program at Children’s Health each year.
We involve a multidisciplinary team including audiologists, speech pathologists, psychologists, and social workers to help you navigate preparing for and adjusting to your new device.
We recommend that you ask your cochlear implant team about device options. There are several types of devices, and no single option is best for everyone. Ongoing research is leading to improvements in cochlear implant technology. Kenneth Lee, M.D., Ph.D., for example, is working on new device designs to improve hearing precision.
You’ll also want to ensure you’ll have access to ongoing rehabilitation and device support to maximize the benefits of your device.
Cochlear implants are one of the most transformative technologies in modern medicine. These small, powerful devices can restore access to conversation, connection, and independence for people who may have spent years struggling to hear.
If you or a loved one might be a candidate for a cochlear implant, don’t wait. Seek an evaluation early – you may have more options than you realize to improve your hearing and quality of life.
To talk with an expert about a cochlear implant evaluation, make an appointment by calling 214-645-8898 or request an appointment online.