When COVID-19 vaccines became widely available, I encouraged everyone I know to get one as soon as they could. Most did, but others needed a few reminders – including my younger brother, Anthony Darrell, who lives in Franklin, Ky., a rural area near the border of Tennessee.
Anthony owns a pool installation company that became increasingly busy during the pandemic. Taking time off to get the vaccine and possibly deal with side effects seemed like an inconvenience, he said.
Unfortunately for Anthony and his family, that one- or two-day potential inconvenience turned into a long and expensive medical ordeal that could have cost him his life.
In early August 2021, Anthony contracted COVID-19 and pneumonia. He spent four days in an ICU in Nashville and was on oxygen support at home for 10 days afterward. He missed several weeks of work and now faces a hefty hospital bill. Doctors also have told him he is facing a long road to recovery. For example, walking to the mailbox still wears him out and he doesn’t know when he can fully return to work.
As much as an older sibling loves to say, “I told you so,” that was the furthest thought from my mind when he called to tell me he was sick. My thoughts immediately turned to worry. For me, it was especially frightening to see someone I love so short of breath. I know from taking care of COVID-19 patients how quickly things can turn deadly, so I immediately flew out to help care for him. I was able to experience COVID-19 care from the other side of the bed, through teleconferences and phone calls with doctors.
Luckily, and with the care of a great medical team, my brother recovered. But it is a long recovery and one we both wish he would have avoided. Anthony has now received his first vaccine dose. So have his wife, their three kids, and many of Anthony’s friends, colleagues, and employees – some of whom might not have gotten vaccinated otherwise.
My brother likes to joke with me that he is more effective at persuading folks to get vaccinated than I am. And frankly, he might be right. I asked Anthony to share his story in hopes it could help more people understand the medical and personal toll COVID-19 can exact on a person and their family – a toll that can be avoided if they get vaccinated.
‘I didn’t think it could happen to me’
The COVID-19 vaccine was definitely on my to-do list, but it just never felt urgent. Social distancing happens pretty naturally here in our small community, and COVID-19 cases had remained relatively low before the Delta variant surged this summer.
My job is physically demanding, and I was working sunup to sundown, so I never made time to go get my shot. Also, I was probably lulled into a false sense of security because I am 41 and have no significant health issues beyond diet-controlled diabetes.
Essentially, I didn’t think it could happen to me.
Delayed diagnosis, serious symptoms
A few days into August, I started feeling sore and overly exhausted. I saw a doctor, but the initial diagnosis was that some dirty diving equipment I’d used while working in a pool the day before had made me sick. I was sent home, but I felt even worse a couple days later and went back. That’s when I tested positive for COVID-19. I was given some pain medication, but I knew I was sick so I called my sister, who is a pulmonary specialist. She had been treating COVID-19 patients at UT Southwestern since March 2020.
Sonja overnighted me a pulse oximeter so I could update her on my oxygen levels, which were dropping pretty fast. She said it might be pneumonia and I needed to go to a hospital, but being the stubborn younger brother, I waited. Within two days, I could barely breathe. My pulse oximeter showed that my oxygen saturations were 85%, and I knew I had to go in. My wife took me to the emergency room, which was an hour away in Nashville.
By the time I sought help, the pneumonia had advanced to a severe stage. I was in the ICU for four days. I received remdesivir and dexamethasone, which have become the standard drugs for patients hospitalized with COVID-19. The doctor told me if this had happened a year earlier, before they had a better understanding of the virus, I would have been on a ventilator.
Related reading: How COVID-19 can put your voice and life at risk

A new reality
A week and a half later, I got to go home but I was still on oxygen. The overall soreness and lack of air were worse than I imagined. I could barely walk to the bathroom without the bottoms of my feet aching, and I had to stop frequently to catch my breath.
Coping with the COVID-19 symptoms – fatigue, body aches, chills – was bad enough; the pneumonia symptoms were the worst part. Every aspect of my life has been negatively impacted.
Family: I saw the worry on my kids’ faces when I arrived at home with an oxygen tank. Isolating from everyone was its own challenge, too. Sonja flew in to help. I stayed in my bedroom, and my wife had to sleep on a mattress in the living room. My illness has been especially hard on her because she covered all my work responsibilities. I lost my voice temporarily, so even when I started moving around without oxygen, I couldn’t take any calls.
Work and finances: My company missed out on a lot of work while I was sick; I can’t even begin to calculate the income lost. I have a small business and I’m self-insured, so I’m likely to end up paying a steep hospital bill.
Health: As of early September, I still hadn’t recovered my sense of smell, and I’ve lost 20 pounds from barely eating or moving for more than a month. Doctors have said it will be a very long time until I feel the way I did before getting COVID-19.
When you don’t have your normal lung capacity, you can’t even yawn without hurting. I would not wish this experience on anyone.
The doctor in the hospital told me that my immune system is so weak right now, I could easily catch another disease that would just knock me out. In a couple of months, I’ll get a chest X-ray to ensure the pneumonia is completely gone before I can be around more people.
Related reading: My COVID-19 action plan: How to cope when the virus hits home
‘Vaccine side effects are nothing compared to the disease’
Now I know there is no good reason not to get vaccinated. The potential side effects are nothing compared to the risks of the disease.
I have now had my first dose of the vaccine and didn’t have any reactions. And the work I was worried about missing because of the vaccine? Well, it was literally nothing compared to the work I have missed due to the debilitating effects of the virus. I am scheduled to get my second dose in late September, and I will be there.
I’ve also told everyone I know to get the vaccine. My family is now fully vaccinated, along with all of my employees – even one who told me a few weeks before I got sick he would never get the vaccine.
What happened to me could happen to anyone. If I didn’t have a sister who was a doctor, and who sent me that pulse oximeter and insisted I go to the hospital, chances are I might not be here right now. And that’s a very frightening thought.
The time is now
Nowadays, Anthony is quick to tell everyone he regrets putting off his vaccination, but many people still share his initial concerns. Even as research on the safety and effectiveness of COVID-19 vaccines continues to grow, only 55% of people in the U.S. – and 50% of people in Texas – are fully vaccinated.
Hesitancy due to a sense of inconvenience, misinformation, persistent myths, and general distrust of government or health care systems puts people who are not vaccinated at risk for serious, preventable COVID-19 complications.
The reality is that if you’re not vaccinated, the virus can multiply more easily and move deeper into your body, increasing your chances of lung damage. A recent CDC study shows that unvaccinated people are:
- More than 10 times more likely to be hospitalized
- And nearly 11 times more likely to die from COVID-19
The vaccine trains your immune system to fight the COVID-19 virus quickly. The faster your system can fight the virus, the less likely you are to get sick.
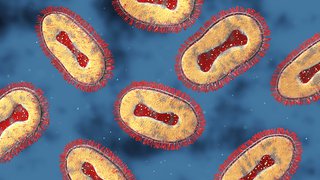
COVID-19 doesn’t affect everyone the same way. Most people experience chills, fever, fatigue, and often a loss of smell and taste. Anthony also got pneumonia, which causes inflammation in the lungs and decreased his ability to take in oxygen. Normal oxygen levels range from 97-99%. Anything in or below the low 90s can be dangerous.

Schedule your free COVID-19 vaccine
If you have yet to receive your protection against COVID-19 and are now ready, UT Southwestern is here for you. Booking an appointment is easy and takes just a few minutes.
Shortness of breath is a good indicator that you have pneumonia, but not everyone with COVID-19 pneumonia experiences this symptom. Using a pulse oximeter to measure your blood oxygen levels can be especially helpful – particularly for people in rural communities who can’t get to a hospital quickly.
Anthony also had a slightly higher risk of getting COVID-19 pneumonia because of his diabetes. Several other medical conditions increase the risk of severe illness from COVID-19, including:
- Cancer
- Chronic kidney or lung diseases
- Dementia
- Heart conditions
- Obesity
- Pregnancy
- Weakened immune system
Even if you do not have these conditions or if you had COVID-19 in the past, don’t put off getting the vaccine – the natural immunity doesn’t last as long as protection provided by the vaccine. Some recent studies suggest that getting vaccinated after having natural COVID-19 can provide a highly protective hybrid immunity against variants.
Bottom line: We hear a lot about the death toll from COVID-19. But more commonly we see patients who recover but experience other long-term effects of the illness. Getting vaccinated can help you avoid the virus-related stress, pain, and financial burdens my brother and his family experienced. Medical and scientific advances have made this prevention possible, so don’t let that privilege pass you by. Listen to your health care team (or your big sister!) and take your shot.