Most patients who contract COVID-19 will recover from the respiratory infection with proper care. But recent data suggest that approximately 20% to 25% of patients may experience significant heart complications due to the body's response to attack the virus.
Chest pain, irregular heart rhythm, and sudden heart weakness appear to emerge approximately two weeks after COVID-19 symptoms surface. In some cases, respiratory symptoms resolve, and then patients are stricken with heart complications.
Compounding this physical reaction is an emotional side effect of the pandemic:
Rampant misinformation, as well as images and data from hard-hit regions, have led to intense fear of catching COVID-19 at the hospital – to the point that patients are avoiding the ER even when they’re experiencing heart attack and other life-threatening symptoms.
Emergency departments around the world have reported major drops in heart attack and heart-related visits. On April 22, eight national cardiology, neurology, and emergency medical institutions issued a "loud and clear" joint statement urging people to understand that it is safe to call 911 and go to the hospital, and that calling 911 offers the best chance of survival during a heart attack or stroke.
The ER at William P. Clements Jr. University Hospital was designed with built-in contingencies to handle pandemic situations. The hospital is equipped with an isolated airflow system in every room, connected to separate ventilation systems within the hospital. Our additional COVID-19 protocols make visiting the ER as safe as – or possibly even safer than – going to the grocery store.
Don't wait when heart attack symptoms strike
More than 800,000 adults in the U.S. have a heart attack every year. That's one person every 40 seconds. COVID-19 has changed many things, but it is highly unlikely that it has made our country’s heart problems disappear.
In fact, COVID-19 is unquestionably adding to the potential for cardiovascular symptoms. We face an unprecedented vicious spiral: COVID-19 infection can provoke serious heart disease. And pre-existing heart disease can make COVID-19 infection worse. Superimposed on this, many people are deferring medical care for fear of contracting the virus.
Since 2018, Clements University Hospital and Parkland Memorial Hospital have been using a highly sensitive cardiac troponin blood test that can determine quickly whether or not someone is having a heart attack. Troponins are proteins released when the heart muscle has been damaged. The test can reduce wait times in the ER, according to a UT Southwestern Study published April 22 in JAMA Open.
COVID-19 is Endangering Our Hearts and Minds
The pandemic is putting stroke and heart attack victims at increased risk as many are staying away from the ER, despite telltale symptoms. UT Southwestern’s Babu Welch, a neurosurgeon, and cardiologist James de Lemos analyze the troubling trend.
If you’re experiencing any of the following, please call 911 or go to the ER:
- Chest pain or discomfort
- Jaw, neck, or back pain
- Lightheadedness or weakness
- Nausea, vomiting, or cold sweat
- Shortness of breath with no apparent cause
- Unexplained arm or shoulder discomfort
Cardiac events, whether they are related to heart attack or a viral attack, limit blood flow to the heart. An inadequate blood supply can kill heart tissue within hours of symptom onset.
And as scary as COVID-19 is, it is important to remember that the likelihood of death from a heart attack without proper medical attention is far higher. Getting emergency care can be the difference between life, death, or living with the complications of heart failure.
What we know about COVID-19 and heart damage
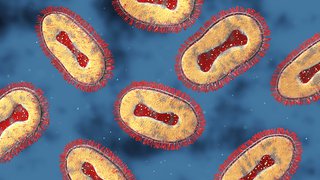
It is likely caused by an extreme immune response to the virus.
When a virus invades the body, the immune system activates inflammation as a defense. Cells, proteins, and fluid flood to the affected area, sometimes causing swelling, redness, or tenderness that typically subside as the body heals.In approximately 20% to 25% of patients with COVID-19, an excessive immune response appears to create a "cytokine storm," in which an overwhelming inflammatory response occurs, releasing into the bloodstream molecules called cytokines. Under normal circumstances, cytokines help regulate the immune response – too many can cause organ failure.
'In 20% to 25% of patients with COVID-19, an excessive immune response appears to create a 'cytokine storm,' which can cause overwhelming inflammation and organ failure.
COVID-19 heart complications tend to arise up to two weeks after infection. These patients' respiratory symptoms begin to resolve but are followed by sudden cardiac distress, such as decreased blood pressure and increased heart rate. In other patients, heart damage may be the first sign of the virus.
Reports out of Italy suggest that more than 40% of COVID-19 cases there were asymptomatic, which presents yet another unprecedented challenge.
The medical community is still learning whether heart damage from cytokine storm can be repaired. However, we know that emergency care can help prevent or reduce heart damage. Come to the ER at the first sign of cardiac symptoms. Protocols are in place to separate patients with COVID-19 from those who are not infected.
Stress and anxiety might cause broken heart syndrome.
During normal circumstances throughout my career, I've seen patients develop anxiety, depression, and even post-traumatic stress disorder, after being diagnosed with cardiovascular disease.
We anticipate this to be true during the pandemic as well. When patients are under a lot of stress, either related to another physical or a behavioral illness, they can develop a condition known as stress cardiomyopathy.
Also known as broken heart syndrome, stress cardiomyopathy causes symptoms similar to heart attack, including sudden heart weakness, chest discomfort, and abnormal breathing. Getting emergency care can reduce the risk of heart failure, severe arrhythmia, or blood clots that could lead to stroke.
There is no way to know at home whether symptoms are related to anxiety or a heart attack. ER doctors and cardiologists will perform specific tests to determine what is wrong and provide appropriate care. If you are concerned about COVID-19 anxiety potentially causing heart problems, contact your doctor.
Diabetes and obesity linked to worse COVID-19 outcomes
Certain conditions, such as heart disease, type 2 diabetes, and obesity, cause inflammation. Chronic inflammation is associated with release of cytokines, which typically assist the immune system. At high concentrations, however, cytokines can damage the heart, the liver, the brain, and more.
Patients with these conditions tend to have worse outcomes with COVID-19 infection. In Dallas County, approximately one-third of hospitalized patients with COVID-19 have had diabetes.
Seeking emergency care for chest pain or discomfort is particularly important for patients who have a chronic condition. Still, many people resist going to the doctor even when we are fortunate to be “on top of the situation” in Dallas.
Related reading: Are stroke sufferers silent victims of COVID-19?
As COVID-19 spreads, telemedicine rises
In March, most of our cardiology patients transitioned to telehealth visits for ongoing checkups and new symptom review. We went virtual with current patients to prevent lapses in care while simultaneously reducing COVID-19 exposure risks to patients and staff.

You can see a heart specialist from home
The COVID-19 pandemic has accelerated access to virtual visits with our cardiologists. If you have questions or concerns about heart disease, video visits are easy to arrange and can be done from the comfort of your home.
Patients and providers quickly adapted to video calls and more extensive use of MyChart electronic medical records. Whereas we cannot use our stethoscopes or perform certain tests, we can ask patients about their symptoms, medications, and converse just like we would in person. If you have a non-emergent problem related to your heart, you can request a virtual visit with our cardiologists who are standing ready to help you. Such telehealth visits are easy to arrange and conduct and can be done from the comfort of your home.
I am certain that COVID-19 has ushered in the next "new normal" of patient-centered care. In addition to outpatient visits conducted virtually, doctors from around the U.S. are being granted temporary license extensions to offer tele-ICU support by interpreting ventilator settings and laboratory data to assist intensive care unit providers in hard-hit areas.
Post-pandemic, I envision further expansion of medical licenses to provide certain aspects of primary and specialist care to patients across the country via mobile devices. In large, highly rural states such as Texas, patients could potentially avoid driving several hours for what might end up being a 30-minute appointment.
A few closing thoughts
As we navigate the next year, the novel coronavirus will no longer be new. But our way of life will undoubtedly be changed forever. We will remember to wash our hands more and touch our faces less. We will try to keep a measurable distance between ourselves and others, at least until a vaccine is created, which is still at least a year away.
Long after the pandemic has passed, there will still be ongoing and emergent medical needs. Medical centers around the U.S. will continue to follow and enhance the protocols we've put in place to ensure that patients are safe from the virus when they enter our doors.
And that is when the lessons learned from COVID-19 will become even more valuable.
Call 911 for emergency symptoms. To visit with a cardiologist for non-emergency symptoms, call 214-645-8300 or request an appointment online.