6 FAQs about COVID-19, pregnancy, and adjusting at home
May 5, 2020

As more data roll in regarding COVID-19, pregnancy and delivery, new questions are surfacing daily from parents.
Last week, Robyn Horsager-Boehrer, M.D., and I held a Facebook Live event to answer on-the-fly questions about how coronavirus is changing the experience of having a baby and adjusting at home.
Many deep questions surfaced during the chat and have come up during regular patient visits. Let's take a look at what patients are asking and what we know about the virus so far.
Related reading: COVID-19 and pregnancy: Answers to 10 key patient questions
1. Are pregnant women more at risk for blood clots due to COVID-19?
We do not yet have substantial data as to whether pregnant women with COVID-19 are at increased risk of developing blood clots.
Emerging data suggest that COVID-19 may activate blood clotting pathways in infected patients. Clotting is one of the body's natural defenses against cell damage. We know that, in some patients, COVID-19 infection can lead to excessive inflammation that damages tissues throughout the body.
However, being pregnant in general increases the risk of developing blood clots. As the uterus expands, it puts pressure on blood vessels in the pelvic area, slowing the return of blood to the heart and increasing opportunities for clots to form. Production of certain clotting factors in the blood are also increased during pregnancy.
Related reading: What all pregnant women should know about blood clots
2. Should patients consider home birth?
The American College of Obstetricians and Gynecologists (ACOG) states that, even during the pandemic, hospitals are still the safest place to give birth. This is particularly true for patients who have risk factors that often require advanced medical support, such as:
- Vaginal delivery after a previous C-section
- A twins or more pregnancy
- Diabetes, gestational diabetes, or high blood pressure
- Heart or other organ concerns
- A fetus in breech position
Even in healthy pregnancies, labor and delivery complications can arise suddenly. Additionally, medical emergencies such as postpartum hemorrhage or neonatal distress require immediate care to avoid serious injury or death.
Still, out-of-hospital births have become increasingly popular in the U.S. over the last decade. Rates increased 59% between 2008 and 2012, according to data published in Obstetrics & Gynecology.
Many women cite increased preferences for natural birth experiences and fewer medical interventions such as cesarean section (C-section). However, to put it all in perspective, only approximately 2% of births occur out of the hospital today.
Related reading: Total body cooling: Saving babies' lives after emergency delivery
Ask the Experts: COVID-19 and pregnancy
Dr. Shivani Patel and Dr. Robyn Horsager-Boehrer answer some of the most frequently asked questions about pregnancy and the novel coronavirus during a recent Facebook interview.
3. Is it safe to breastfeed my baby if I've had COVID-19?

To date, there is no known data to determine whether the virus can be transmitted from mother to baby through breast milk.
There is potential for transmission of antibodies – blood proteins that help the immune system defend against foreign substances in the body, such as viruses – through breast milk. However, there is not enough COVID-specific data to know for sure just yet.
ACOG and the Centers for Disease Control and Prevention (CDC) still recommend that mothers provide their babies with breast milk through breastfeeding or pumping and bottle feeding. Now is a good opportunity to develop a good pumping routine if you work outside the home or plan to after the pandemic.
If you have COVID-19 or have recently recovered, consider pumping and asking your partner or another caregiver to bottle feed the baby. If this is not an option, wear a face mask while nursing and wash your hands thoroughly before and after each feeding. A breastfeeding cape may help protect your baby as well.
4. Is it safe to get prenatal care at a hospital or doctor’s office?
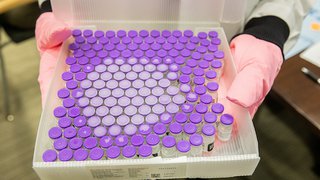
Yes. All patients and visitors are screened for symptoms before entering the hospital, and all patients at William P. Clements Jr. University Hospital are tested prior to entering the labor and delivery unit.
That said, we are moving much of our prenatal care to telehealth to make access to care easier for patients and to reduce the number of people in the hospital during the pandemic.
Patients who don't need labs or a physical exam can often use MyChart, phone calls, or secure video telehealth visits to meet with their provider. Even phone visits with your provider can be valuable. Women with high-risk pregnancies typically require more in-person visits to monitor their health and that of the baby.
Related reading: Visitors, doulas, and video calls: Birth plan updates during the COVID-19 pandemic
5. What should pregnant patients do if they need urgent care?
Some pregnancy symptoms can be mistaken for coronavirus symptoms, including labored breathing late in the pregnancy.
However, we encourage you to call your provider with any concerning symptoms. It is always better to ask about symptoms than to worry on your own. Your provider may suggest you come to clinic or direct you elsewhere, like the emergency room.
Related reading: Top symptoms patients might not expect during pregnancy
6. How can partners be extra supportive right now?
While partners can't take on the physical challenges of pregnancy, there are many ways they can support their loved one during this stressful time.
A colleague at UT Austin created an app called Father's Playbook, which offers pregnancy information for expecting dads. The app also offers tips for partners to pitch in with financial planning, infant CPR, and registration for the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Learn more.

Partners should take extra precautions to reduce coronavirus exposure risks, such as wearing a mask in public and washing their hands regularly. Partners might also volunteer to do the grocery shopping so mom-to-be can avoid exposure at the store.
Handling pet waste and medication duty is another great way to help. Chemicals in flea and tick repellent and kitty litter can be harmful to mom and baby. Also, partners can lend a listening ear if mom is worried. It's normal to have fears and concerns in uncertain times. Sometimes just having someone listen without judgment can help alleviate stress.
After the baby is born, there will be new concerns, such as having visitors at home and keeping toys and surfaces sanitary. Partners can help with selecting safe products to use at home, as well as helping keep the house clean.
As we learn more about the novel coronavirus, we will be able to answer more of the unknowns. For now, pregnant patients and their partners should feel empowered to reach out to their provider with questions. We are all in this together and, as always, our goal is to help you have a healthy, happy pregnancy.
To visit with an Ob/Gyn, call 214-645-8300 or request an appointment online.