Risk Factors
Risk factors for cardiac arrhythmias vary, depending on the particular type of rhythm disorder. Some of these, such as family history/genetics and age, are not modifiable. However, beneficial lifestyle changes to address risk factors for overall cardiac disease, such as obesity, sleep apnea, inactivity, diabetes, smoking, excessive alcohol consumption, and hypertension, can reduce the risk for AFib.
Symptoms
Symptoms from arrhythmias are highly variable. They include palpitations, skipping, fluttering, lightheadedness, fatigue, chest pain, and difficulty breathing.
Many people have palpitations that may raise concerns about a possible heart rhythm disorder. Such palpitations may be caused by too much caffeine (including that found in chocolate), alcohol, nicotine, stress, exercise, dehydration, or by an abnormal heart rhythm. Even when palpitations are caused by a heart rhythm disorder, most aren’t dangerous.
However, if a patient has palpitations accompanied by chest pain, lightheadedness or dizziness, shortness of breath, sweating, or fainting, he or she should seek immediate medical attention. To be safe, consult our doctors if experiencing any of these symptoms:
- A feeling that the heart is skipping a beat
- A heartbeat that is too fast or “racing”
- A heartbeat that is too slow
- An irregular heartbeat
- Pauses between heartbeats
Diagnosis
Cardiologists who specialize in the treatment of heart rhythm disorders, known as electrophysiologists, use many techniques to evaluate the condition and determine the best treatment procedures, devices, or medications. Tests that may be performed to diagnose arrhythmia include:
- Electrocardiogram: Measures heart rate, heart rhythm, and strength of electrical signals in the heart
- Event monitoring: Records and transmits heart patterns using a small, pager-sized device that records electrocardiogram patterns when activated by the patient. Patients can wear these for up to 30 days.
- Holter monitor: An external device worn by the patient that records a 24-to-48 hour continuous ECG of the heart's electrical activity
- Implantable loop recorder: A small recording device that is inserted under the skin and monitors the heartbeat for up to five years
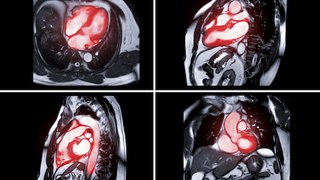
- Echocardiogram: Produces a moving picture of the heart, using a device called a transducer that is placed on the chest
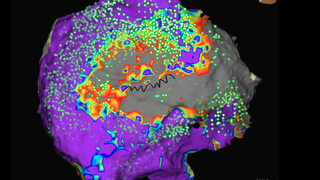
- Electrophysiology study: Insertion of a specially outfitted catheter close to the heart to measure electrical impulses, pinpoint injured heart muscle, and administer electric impulses to evaluate arrhythmias
- Cardiac stress testing: Evaluates how the heart performs during exertion, such as walking on a treadmill or riding a stationary bike
- Wearable monitors: Increasingly, consumer products such as the Apple Watch, Alive Cor, and Fitbit can record an ECG. While these are not as accurate as medical-grade monitors, they still can be useful in making a diagnosis.
Treatments
UT Southwestern’s multidisciplinary approach offers our patients the best opportunity for longer and healthier lives. Patients and their families receive clear, comprehensive information about the risks and benefits of all treatment options. We then create a treatment plan tailored to each patient’s condition, needs, and goals.
If medications cannot be tolerated or do not significantly reduce arrhythmias, patients may be a candidate for one or more minimally invasive heart rhythm management procedures. UT Southwestern cardiology specialists are renowned for their expertise in these procedures, which include:
- Catheter ablation: Delivery of focused energy to specific areas of the heart to produce a tiny scar that blocks irregular impulses, curing or minimizing abnormal heart rhythms in many patients
- Electrical cardioversion: Delivery of an electric current to the chest so that the heart’s rhythm is reset to normal
- Implantable cardioverter defibrillator (ICD): A small electronic device that is implanted under the skin to continually monitor heart rhythm and deliver an electric current that can regulate or reset the heart’s rhythm as needed. At UT Southwestern, both transvenous and subcutaneous ICDs are available.
- Implantable pacemaker: A small, battery-operated device surgically placed under the skin that can sense heart rhythms and send electrical impulses through the heart to regulate, increase, or decrease the heartbeat as needed
- Leadless implantable pacemaker: The next generation of pacemaker technology, the leadless pacemaker is placed directly in the heart without any leads. This eliminates wear-and-tear on leads and reduces infection risk.
- Cardiac resynchronization treatment (CRT): Placing an additional lead on the outside of the left ventricle may improve heart failure symptoms and quality of life for individuals with heart failure, low ejection fractions, and conduction disease.
- Left atrial occlusion devices: These devices can reduce the risk of stroke for patients with AFib who can’t take anticoagulants.
For some people with atrial fibrillation, a combination of medications or procedures may be needed to prevent rapid or slow heart rates, restore and maintain normal heart rhythm, and prevent strokes.
Aggressive treatment of other health conditions that may contribute to heart arrhythmias or make them more dangerous, such as sleep apnea, diabetes, and hypertension, can also help improve the overall health of people with arrhythmias such as atrial fibrillation.
Both implantable cardioverter defibrillators and pacemakers may get infected. Infected devices generally need removal. Removal of a device is much riskier than implantation. Surgeons and electrophysiologists at UT Southwestern have safely performed thousands of these removal procedures. Learn more about lead extraction.