Transformational Leaders in Patient Care
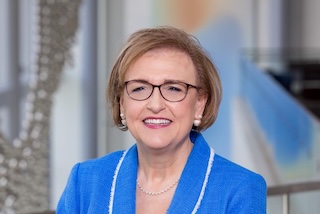
"As I walk the halls of our University Hospital and clinics each day, it's no wonder I smile. Around every corner, I see reflections of nursing at UT Southwestern; it's often in the greeting of a grateful patient. The patient experience drives us in our calling as nurses. Nurses here are passionate about patient care excellence. They make sure that the whole family unit feels cared for and part of the team. They are transformational leaders at every level."
– Susan Hernandez, D.N.P., M.B.A., RN
Chief Nurse Executive, UT Southwestern Health System