Clinical trials are crucial in the evaluation and development of new medical treatments for cancer. Participating in a clinical trial is a powerful way to be part of finding new, more effective treatments.
Breast cancer is the most common cancer in women and will affect one in eight women during her lifetime. At UT Southwestern, we offer multidisciplinary care, including a breast-specific tumor board, that brings all specialists under one roof to devise the best treatment plan for each patient. Our breast cancer team, led by Asal Rahimi, M.D., also offers multiple cutting-edge radiation clinical trials.
What sets us apart?
- We have the most comprehensive deep inspiration breath hold (DIBH)-based cardiac-sparing radiation treatment program in North Texas for patients with left-sided breast cancer.
- The GammaPod is the first stereotactic body radiation therapy (SBRT) system optimized for treating breast cancer. By using principles of stereotactic radiotherapy to deliver higher doses in one to five treatment fractions, GammaPod can both reduce treatment time and potentially lower the toxicity of treatment. Learn more about the GammaPod.
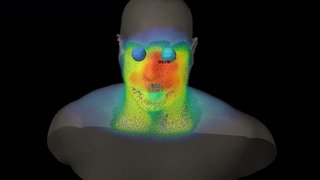
- Two Vision RT surface image-guided systems dedicated for patients requiring left breast radiation treatments.
- Two Active Breathing Coordinator (ABC) machines used to monitor patients requiring breast/chest wall and lymph node treatments.
- Ongoing, active research in deep inspiration breath hold (DIBH)-based cardiac-sparing radiation treatment delivery.